Let’s begin Cleft lip and palate in detail.
Definition of Cleft
The dictionary defines cleft as a crack, fissure, split or a gap
Nomenclature of Orofacial clefts
- Earlier termed as LAGOCHEILOS, meaning hare lip.
- Galen, in 120-200 AD, coined the term.
- However, now they are referred to as cleft lip & cleft palate.
Definition of Cleft Lip
It is a congenital disability that results in a unilateral or bilateral opening in the upper lip between the mouth & the nose.
Definition of Cleft Palate
It is a birth defect characterized by an opening in the roof of the mouth caused by a lack of tissue development.
“A congenital fissure or an elongated opening in the soft or hard palate.” (GPT-8)
“An opening in the hard and/or soft palate due to improper union of maxillary process & the median nasal process during the 2nd month of intrauterine development.” (GPT-8)
Epidemiology of Cleft lip and palate
Cleft lip & palate are the most prevalent developmental disorders of the orofacial structures.
A cleft lip can occur with/ without cleft palate and is denoted by CL(P).
When cleft palate occurs alone, it is referred to as a Cleft lip.
The racial predilection for CL(P)
- Negroes – 1 in 3000 live births (Altemus et al, 1966; Davis, 1924; Ivy, 1957)
- Caucasians – 1 in 750 live births (Greene et al, 1964; Sesgin et al, 1961)
- Mongoloids – 1 in 500 live births (Neel, 1958)
- Indians – 1 in 862 live births
Racial predilection for CP
- Negroes – 1 in 5000 live births
- Caucasians – 1 in 3000 live births
- Mongoloids (Japanese) – 1 in 2000 live births
- Indians – 1 in 2325 live births
Sex Predilection for Cleft lip and palate
CL(P) is more common in males as compared to females.
(Fraser et al, 1961; Loretz et al, 1961; Mazaheri, 1958)
CP is more common in females as compared to males.
(Fraser et al, 1961; Greene et al, 1964; Mazaheri, 1958)
No explanation is available for this
Birkenfeld (1926) & Fogh Andersan (1942) have reported that
Isolated CL – 25% cases
Isolated CP – 25 % cases
CL(P) – 50 % cases
Lip clefts have a preference of the left side in the ratio of 2:1 in CL & CL(P)
A bilateral isolated cleft lip is rare & comprises only 6-7 % of all isolated cleft lip (CL) cases.
Older mothers have a higher risk of bearing a cleft child.
(Macmahan & Mckeown, 1953; woolf et al, 1963; Fraser & Calnan, 1961)
No influence of paternal age on the frequency of clefting has been reported.
Seasonal Distribution
Higher incidence in spring & lower rate in summer.
(Fujino et al in Japanese population)
Classification of Cleft lip and palate
Various classification systems have been supported
- Davis & Ritchie (1922)
- Veau (1931)
- Fogh Andersan (1942)
- Karnahan & Stark (1958)
- Harkins et al (1962)
- Internationally approved classification (1967)
- Karnahan’s classification – The ‘Y’
- Nabil Elsahy Modification
Davis & Ritchie – Anatomical Classification
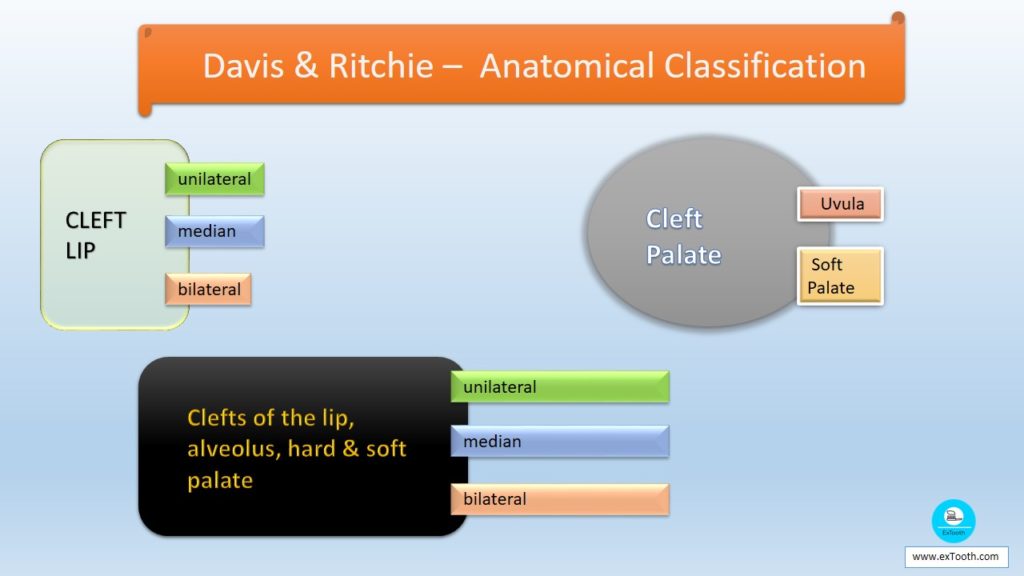
Group I – Cleft lip
I – 1 — unilateral
I – 2 — median
I – 3 — bilateral
Group II – Cleft Palate
II – 1 — Uvula
II – 2 — Soft Palate
Group III – Clefts of the lip, alveolus, hard & soft palate
III – 1 — unilateral
III – 2 — median
III – 3 — bilateral
Veau
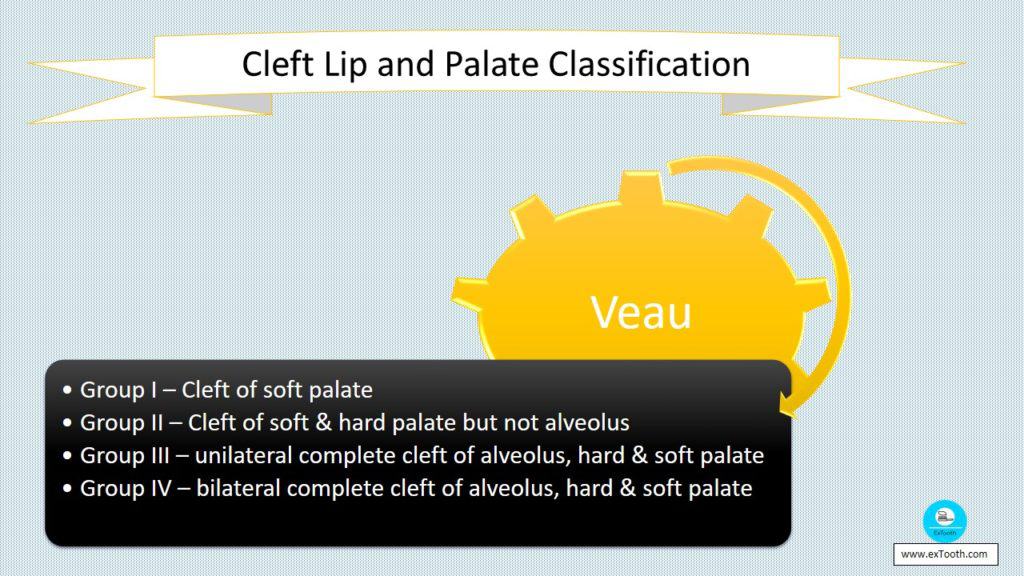
Group I – Cleft of soft palate
Group II – Cleft of soft & hard palate but not alveolus
Group III – unilateral complete cleft of alveolus, hard & soft palate
Group IV – bilateral complete cleft of alveolus, hard & soft palate
Fogh Andersan – Morphologic Classification
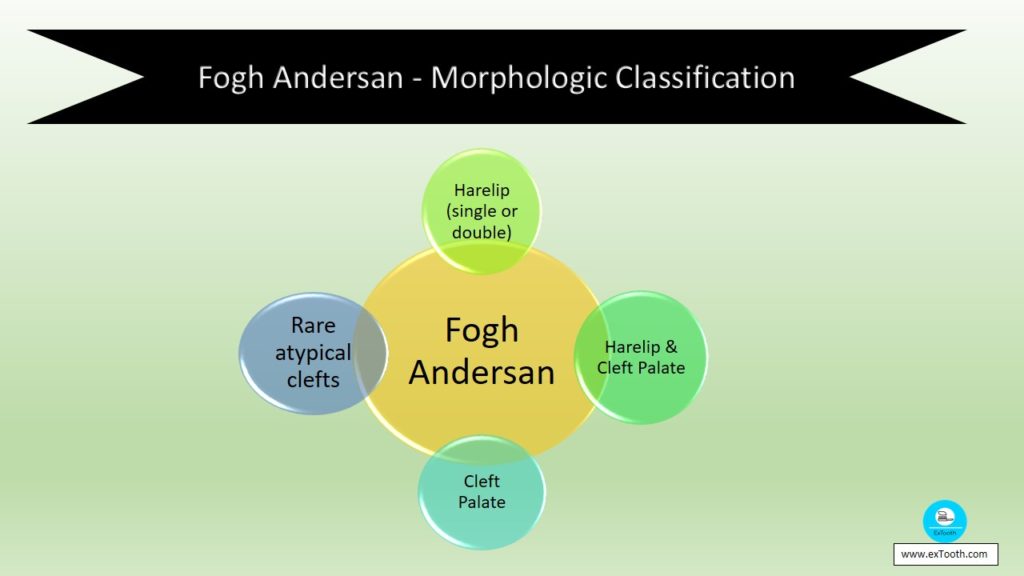
Harelip (single or double)
Harelip & Cleft Palate
Cleft Palate
Rare atypical clefts
They described something called as Submucous clefts. There is a cleft in the hard palate, but the palatal mucosa is intact & covers it.
Kernahan & Stark – Embroyological basis
- Clefts of primary palate – clefts of lip & premaxilla occurring at 4-7 weeks of embryonic life.
- Clefts of secondary palate – clefts of hard & soft palate posterior to the incisive foramen occurring at 7-12 weeks.
Internationally Approved Classification
Group I – Clefts of anterior (primary) palate
Lip – right and/or left side
Alveolus – right and/or left side
Group II – Clefts of anterior & posterior palate
Lip – right and/or left side
Alveolus – right and/or left side
Hard palate – right and/or left side
Group III – Clefts of posterior (secondary palate)
Hard palate – right and/or left side
Soft palate – right and/or left side
Rare facial clefts
Kernahan – The ‘Y’
1 & 4 – Lip
2 & 5 – Alveolus
3 & 6 – Area of hard palate from alveolus to incisive foramen
7 & 8 – Hard palate
9 – Soft palate
Nabil Elsahy modified the ‘Y’
1 & 5 – nasal floor
2 & 6 – Lip
3 & 7 – Alveolus
4 & 8 – Area of hard palate from alveolus to incisive foramen
9 & 10 – Hard palate
11 – Soft palate
12 – Pharynx
13 – Premaxilla
Etiology of Cleft lip and palate
- Hereditary
- Polygenic inheritance
- Monogenic (syndromic inheritance)
- Environmental
Hereditary
Fogh Andersen in 1942 have shown that there is a 40 % chance of occurrence if there is a familial history of cleft lip and palate, while 18-20 % chance of isolated cleft palate
The various hypothesis has been presented to explain this. These include
Polygenic inheritance
widely accepted
Mode of transmission is through several genes each producing a small effect which together creates this condition (Bhatia 1972)
Monogenic (syndromic inheritance)
Less widely accepted
One gene is responsible for the cleft
Associated with various syndromes (150) like
Van Der Woude Syndrome
Pierre Robin Syndrome
Treacher Collins Syndrome
Oral Facial digital Syndrome, etc Bixler (1975)
Environmental Factors
- 80 % of cases of clefts are due to environmental influence or due to teratogenic agents
- Various factors which influence the incidence of Cleft lip and palate during 1st trimester of pregnancy are
- Viral infection (Buchner,1959)
- Exposure to radiation
- Anemia
- Anorexia
- Influence of drugs like antibiotics, steroids, insulin & antiepileptic drugs
- Deficiency of Vitamin A, riboflavin, Folic acid, Pantothenic acid. (Warkany et al 1955)
- Stress as it increases cortisone secretion (Streen & Peer, 1958)
- Excessive consumption of alcohol
- Excessive tobacco chewing & smoking
- Consanguineous marriages
- Increased maternal age as there is a chance of defective zygote &
- Decreased vascular supply to the area
Buchner in 1959 has stated four principal environmental factors for nonfamilial facial clefts.
- Acute viral infection
- Avitaminosis
- Oxygen deprivation
- Glucose deprivation
Embryology
The face is formed by the
frontonasal process,
stomatodeum &
the 1st pharyngeal (mandibular) arch of each side.
Mandibular arch yields off a bud from its dorsal end called the maxillary process.
It grows ventromedial & cranially to the central part of the arch which is now called as the mandibular arch
Ectoderm overlying the frontonasal process shows bilateral localized thickening above the stomatodeum called as nasal placodes
These placodes sink below to form nasal pits
The edges of these pits are raised above the surface.
The medial edge is called the medial nasal process
The lateral is called the lateral nasal process
Embryology – Lower Lip
The mandibular processes of the two sides grow towards each other & fuse in the midline to form the lower lip & the lower jaw
Embryology – Upper lip
Each maxillary process grows medially & fuses with the lateral nasal process & then with the median nasal process.
The median & lateral nasal processes also fuse
Embryology – Upper lip
The frontonasal process considerably becomes narrower due to the growth of the maxillary process so that the two nares become close to each other.
Embryology – Upper lip
The stomatodeum is now bounded above by the upper lip which is derived as follows
Medial part from the frontonasal process
Lateral part from the maxillary process
Embryology – Palate
The frontonasal process forms the primary palate.
The secondary palate is formed by two shelves, like outgrowths from the maxillary process.
These palatine shelves appear in the 6th week of intrauterine life & are directed on either side of the tongue downward & obliquely.
In the 7th week, the palatine shelves ascend to attain a horizontal position above the tongue & fuse together to form the secondary palate
Anteriorly the secondary palate fuses with the triangular primary palate & the incisive foramen are formed at this junction between 7th & 10th wks of development.
At the same time, the nasal septum grows downwards & joins the superior surface of the newly formed palate.
At a later stage, the mesoderm in the palate undergoes ossification to form the hard palate.
Ossification, however, does not extend to the posterior part, which forms the soft palate.
Pathogenesis
Various theories have been put forward to explain clefts. These include
- Theory of Dursy-His
- Philosophy of failure of mesodermal migration
- Merging
- Others
However, no theory enjoys universal acceptance
Theory of Dursy-His
- Dursy & His popularized the theory of embryologic development of midface by the fusion of 5 facial processes about the stomatodeum.
- These included
- Frontonasal process
- Paired maxillary process &
- Paired mandibular process
- According to this classical theory, all of these processes grow forward as finger-like projections to fuse to form the regular face between the 5th & 8th wks.
- The failure of fusion of these processes explained the formation of various degrees of clefts.
- This theory reigned for 30 yrs but is no longer in vogue.
Theory of Failure of Mesodermal Migration
Proposed by A. Fleischmann in 1910.
It proposes that coincidental with the invagination of the oral cavity & nasal pits; there is heaping up of adjacent tissue forming facial prominences.
As the nasal & oral cavities deepen, there is an increase in the size of these prominences due to the penetration of mesoderm.
As more mesoderm enters the area, the bulging effect is increased, leading to the formation of hills & valleys (prominences & grooves).
The difference between a hill & a valley is merely dependent upon the amount of mesoderm between the two epithelial layers.
As these prominences approach each other, their blending is at the expense of the valleys (grooves).
Failure of sufficient mesoderm to migrate into a particular area would be responsible for the persistence of a groove.
With the following epithelial breakdown, the persistent groove gives rise to an established cleft.
Merging
- Proposed by Bradley Pattern
- Combined the fusion & migration theories.
Other Theories
Various Authors have put forth their theories. Some of them include
- Tondury (1950) – Failure of the epithelial wall to develop
- Steininger (1939) – rupture of previously formed cysts in the soft tissue bridges.
- Pfeiffer (1966)
Clinical Features
- Difficulty in sucking
- Difficulty in eating & drinking
- Nasal regurgitation
- Speech difficulties with consonant sounds (p, b, t, d, k, & g).
- Infections
- Hearing loss
- Unpleasant appearance
- Dental problems
- Congenitally absent/supernumerary teeth
- Crowding or displacement of permanent teeth
- Hypomineralised teeth
- Hypoplastic maxilla results in pseudo mandibular prognathism
- Narrow arch form due to the constricted maxilla
- Psychosocial problems
Diagnosis
- Case History
- Study casts
- Radiographs
- Cephalogram
- Full mouth IOPA’s
- Bitewing radiograph
- Occlusal radiograph
- Cineradiography
- Laminography
- Photographs
- Speech recording
- Sound spectrographic recordings
- Measurement of nasal & oral pressure & flow
- Otologic & Hearing examination
- Study casts, radiographs & pictures are to be made by the dentist at birth, & then semiannually till the child is two years old. After two years of age, all of these are made once every year.
Management of Cleft lip and palate
Clefts of primary & secondary palate present a complex biologic, sociologic & psychologic problem one whose best management involves several disciplines through a team approach.
Team members include,
- Pedodontist
- Surgeon
- Oral surgeon
- Orthodontist
- Prosthodontist
- Speech Therapist
- Psychiatrist
- Social worker
Aims & Objectives of treatment
- To improve the birth defect surgically so that the patient can have pleasant facial esthetics.
- To allow clear communication
- To correct the dentition to allow regular function & looks.
General Management protocol
- At Birth
- Pediatric Consultation
- Counseling
- Feeding instructions & management
- Evaluation by geneticist
- Diagnosis of life expectancy of a child
- Diagnostic tests
- Within a few weeks of life
- Team evaluation including hearing testing
- 10 -12 weeks
- Surgical repair of lip
- Before 12 to 18 months
Team evaluation
- Surgical repair of cleft palate & placement of pressure equalization tubes
- Three months after palate repair
Team evaluation for speech & language assessment
3 – 6 years
Team evaluation
- Behavior Management
- Speech therapy
- Treatment for middle ear infection
- Fistula repair
- Soft palate lengthening
- Orthodontic treatment – Phase I
- Psychological evaluation
- 5-6 years
Lip, nose revision if necessary
Pharyngeal surgery
Seven years
Orthodontic treatment – phase II
9 -11 years
Pre-alveolar bone grafting
After 12 Years
Full orthodontic treatment – phase III
15 – 18 years
After orthodontic treatment, placement of implants, fixed bridge, etc
16- 18 years
Final rhinoplasty for nose & lip revision if surgical advancement of maxillae not required.
18- 21 years
When growth is completed, surgical advancement of maxilla if needed.
Management of Feeding Problems in Cleft lip and palate
Feeding is one of the 1st experiences in an infant’s life.
For infants & their parents, such experiences should produce feelings of contentment & security rather than tension, stress, & fear.
Effective teaching of successful feeding habits is one of the most significant challenges faced by the professionals treating a cleft patient.
Assessment by a feeding specialist within 24 hrs of birth
Breastfeeding is the preferred choice. If necessary supplementary feeds can be given with a spoon, cup, or scoop bottle.
If breastfeeding is unsuccessful & the baby requires supplementation, the use of expressed breast milk is the second option, but it requires a breast pump.
The use of a feeding plate helps the baby to suck effectively.
Another option is bottle feeding.
While bottle-feeding, the teat is placed well into the baby’s mouth & is kept as still as possible while the baby suckles.
Movement of the teat may cause ulceration of the nasal septum & the nasal turbinates
Arvedson in 1993 has recommended that the baby should be fed comfortably cradled in the parent’s arm with the head & upper body well supported, & the chin midway between flexion & extension
The feed should be completed within 30-40 minutes with minimum ingestion of air.
Assisted feeding
Enlarging the existing hole in a latex teat
Making an additional hole in the teat
Use of above with a soft, flexible bottle
The smooth bottle is gently squeezed as the baby suckles, compensating for the oral stage difficulty
Feeding plate
It has been suggested that the use of a feeding plate helps the baby in sucking.
However, Herzog-Isler in 1994 has stated that feeding plates are unhelpful & unnecessary in bottle feeding.
If correctly made and fitted they seem to have limited use as a breastfeeding aid
Impression obtained with the infant fully awake and without any anesthesia
Position – Infant face down, head gently held in a slightly upright position
Materials for making impression include
Impression compound
Alginate
Silicone
Role of Surgeon in Cleft lip and palate treatment
- Cleft Lip
- The timing of surgery for cleft lip varies from the first 48 hrs of life to 6 months of age, depending upon the surgeon’s judgment.
- Most surgeons follow Millard’s rule of 10. i.e., ten weeks of age, 10gm of Hb, 10 gm of weight.
- Cleft palate
- Again there are various schools of thought regarding the timing of repair.
Chalian has recommended a group of arbitrary criteria to determine the optimal time of surgery. These include,
- Child should be free of any systemic or local disease.
- Child must have a minimum weight of 7 pounds
- Chalian has recommended that primary repair of the palate should be done at approximately 18 months of age except in the case of complete bilateral cleft of palate.
- For complete bilateral clefts of palate, a two-stage procedure with the 1st surgery at 12-15 months while the 2nd three months later is recommended.
Role of General Dentist/ Pedodontist in Cleft lip and palate treatment
Behavior management
Transpalatal arch – to prevent the collapse of posterior segment.
Preventive care –
Teaching parents how to brush their child’s teeth.
Use of disclosing tablet while tooth brushing
Use of dental floss
Restorative care
Steel crowns / cast gold crowns on hypoplastic teeth.
Restoration of carious lesions
Acrylic crowns on anterior teeth during mixed dentition phase.
Role of Orthodontist in Cleft lip and palate treatment
- Orthodontic treatment is done in 3 phases
- Phase I –
- Early posterior segment alignment following the eruption of full complement of deciduous molars.
- Done at the age of 3 – 5 years
- Appliances used are
- Fixed lingual arch
- Removable lingual arch
- Split palate with jackscrew
- Phase II –
- Posterior & anterior segment alignment in early mixed dentition or late primary dentition.
- Also, correction of traumatic occlusion is done
- Done at the age of 5 – 7 years
- Phase III –
- Comprehensive orthodontic treatment to correct the malocclusion.
- Done after 12 years of age
Role of Prosthodontist
- Pre-surgical
- Feeding Plate
- Presurgical infant orthopedics (PSIO)
- Presurgical Nasoalveolar Molding (PNAM)
- Surgical
- Post-surgical
- Speech Prosthesis
- Fixed Partial Denture
- Removable Partial Denture
- Overlay denture
Aim of Prosthodontic treatment
- To improve appearance
- To provide adequate function including speech
Presurgical Infant Orthopedics
Also called mold plate therapy
Introduced by McNeil in 1950.
This procedure has aided significantly in reducing the size of the clefts of alveolus & hard palate before surgery
However, it has been surrounded by controversy in conjunction with various surgical protocols when employed to move only the anterior segments closer together.
Two types of appliances are used
Passive or holding appliance – Used when there is no collapse of palate
Active or expansion appliance – Used when there is collapse of palate
However, if collapse is only in the anterior segment the a fan type of split holding appliance can be used
If a holding appliance is used, then surgery for cleft lip can be carried out.
In cases of arch collapse, surgical closure of lip is delayed until the expansion appliance has achieved an ideal arch configuration.
The primary purpose of the appliance before lip closure is not to increase tissue & initiate growth but to guide the maxillary segments into proper spatial position with each other & the mandible.
The molding pressure of the surgically closed-lip & the appliance helps to create an ideal arch form.
Presurgical Nasoalveolar Molding
Developed at the Institute of Reconstructive Plastic Surgery at New York University Medical center.
PNAM (Presurgical Nasoalveolar Molding) includes not only reduction of size of the alveolar cleft through molding of bony segments but also the active frame & positioning of surrounding soft tissues, including the deformed soft tissue & cartilage in cleft nose
This is accomplished with the use of a nasal stent.
The stent provides support & gives shape to the nasal dome & alar cartilages.
It can successfully be employed for early management of both the unilateral & bilateral cleft anomalies in newborn.
Correction of Unilateral Oronasal Cleft
Impression made with heavy body elastomeric material.
Wash with light body not made as minute details are not required.
Alginate is not used because of weak tear strength, the chance of pieces occluding the air passages & inavailability to obtain two casts from a single impression
Impression obtained with the infant fully awake and without any anesthesia
Position – Infant faces down to prevent aspiration & head gently held in a slightly upright position. Infant should be able to cry during impression making. If no crying is heard, then airway is blocked.
Impression is removed when the material has set & poured twice in modified dental stone.
One cast serves as a working cast to fabricate the molding device while the other becomes part of patients permanent record.
The cleft region can be filled with wax to approximate the contour & topography of the intact arch
A soft, resilient, slowly polymerizing acrylic may be applied in the undercut regions of the cast while the remaining molding plate is fabricated from clear methyl methacrylate.
Either self cure or heat cure material can be used.
The plate is then finished & polished.
The oral molding appliance is checked in the child’s mouth for border extensions & retention.
The tissue surface of the appliance is modified at the initial appointment to begin molding of the greater & lesser alveolar segments on either sides of the cleft.
This is achieved by weekly minor adjustments like
selective removal of acrylic from the region into which one desires the bone to move.
Soft resilient acrylic (Permasoft) is added to line the appliance in the region from which one desires to move the bone.
Proper taping serves to retain the appliance.
Also, it functions much like lip adhesion that allows the soft tissues of the lip & nasal base regions to become more properly oriented as the nasal stent is developed.
Lip adhesion alone produces uncontrolled orthopedic effects while lip taping force in conjunction with a molding plate yields a controlled movement of the alveolar segments.
Addition of nasal stent
When cleft gap has been reduced to approx 6 mm or less, a nasal stent may be added to the appliance.
Thus the stage of active nasal cartilage molding begins.
The nasal stent can be made by addition of small increments of acrylic resin until the stent is positioned inside the nasal dome on the cleft side of the nose.
It can also be made by extending a 0.036 inch stainless steel wire from the labial flange to inside the nostril with the end covered by clear acrylic which in turn is covered by a soft resilient resin.
If the appliance has been properly modified, adapted at each visit & used continuously, alveolar segments come in contact after 4 – 6 weeks of oral molding plate therapy.(< 10 mm clefts).
The goal of nasal orthopedics is to ensure that when the lip segments are drawn together with taping, the columella has been positioned to a midline location or even overcorrected prior to surgery
Correction of Bilateral Oronasal Cleft
Nasoalveolar molding of bilateral cases of cleft produces expansion of skin of columella & the nasal lining tissues.
Nasal cartilage is also molded presurgically while the premaxilla is retracted into a normal position.
In Bilateral cases PNAM consists of 3 phases
1st phase – intraoral phase –
Alignment of posterior lateral alveolar segments while retracting & derotating the premaxilla.
2nd phase –
Molding of nasal cartilages by repositioning the apices of the alar cartilage toward the nasal tip.
3rd Phase – Elongation of columella
Impressions are recorded in heavy body silicone.
Clear acrylic intraoral molding plate is fabricated with 2 retentive buttons.
Correction of Bilateral Oronasal Cleft
Two separate elastics with tapes are used to retain the bilateral molding device.
Adjustments have to be made more than once a week in the initial molding period
After the premaxilla attains a reasonable position (3-4 weeks), the nasal molding phase of treatment begins.
2 nasal stents are built
As the position of the nasal cartilages normalises, the last phase of molding is introduced.
The appliance is modified again by attaching a horizontal prolabial band or saddle across the two acrylic nasal stents.
The band pushes back against the base of the columella & directs the expansion forces to preserve the nasolabial angle.
This eventually leads to elongation of the columella.
Nasoalveolar molding with columellar elongation requires up to 5-6 months.
Prosthetic Speech Appliance
- Indications in Unoperated palates
- Wide clefts with deficient soft palate
- Wide cleft of hard palate
- Neuromuscular deficiency of soft palate & pharynx
- Delayed surgery due to medical reasons
- Expansion prosthesis to improve spatial relations
- Combined prosthesis & orthodontic appliance
- Indications in operated palates
- An incompetent palatopharyngeal mechanism
- Surgical Failures
Contraindications for prosthesis
- Mentally retarded patient as he cannot take care of the prosthesis.
- For an uncooperative patient or a patient with uncooperative parents.
- In cases of rampant uncontrolled caries.
- When experienced Prosthodontic help is unavailable.
Requirements of speech appliance
The prosthesis should be designed for the individual patient in relation to his oral & facial balance, masticatory function & speech.
Preservation of the remaining dentition & surrounding soft and hard tissue is of utmost importance
It should have more retention & support than most other restorations
Mouth preparation should be completed before making final impressions.
Weight & size of the prosthetic speech appliance should be kept to a minimum.
Material used should be easy to repair, extend & reduce.
Soft tissue displacement in velar & nasopharyngeal areas by the prosthesis should be avoided.
Velar & pharyngeal sections of the prosthesis should never be displaced by lateral & posterior pharyngeal wall muscle activities or tongue movements during swallowing & speech.
The upper part of the pharyngeal region should be sloped sideways to reduce the accumulation of nasal discharges.
The lower part of the pharyngeal region should be somewhat sunken to provide for ease of tongue action.
The speech bulb should be placed in the area of the greatest posterior pharyngeal & lateral pharyngeal wall activity since the voice tone is heard completely when the speech bulb is at these sites.
The inferior-superior dimension & weight of the speech bulb may be decreased
Prosthetic Speech Appliances for Children
5 types
- Obturator with a palatal-velar-pharyngeal portion
- Meatal obturator
- Palatal Lift Prosthesis
- Baseplate type which functions to obturate the palate & helps speech.
- Anterior prosthesis
Obturator with a Palatal-Velar-Pharyngeal Portion
Used as a training, diagnosis & as a temporary appliance.
Rationale of pharyngeal bulb – it acts within the nasopharynx to allow complete velopharyngeal closure during speech & yet presents an open velopharyngeal port for breathing.
Construction of Pharyngeal Bulb
- The bulb is constructed in increments of compound starting with a small bulb about the size of a pea.
- With each increment the child is asked to bend his head down as far as he can as this brings the spinal column forward, causing the posterior pharyngeal wall to indent the posterior surface of the impression.
- Next, the child moves his head from side to side, which causes the palatopharyngeus muscle to trim the anterolateral aspects of the bulb.
- Once adding of material is completed, thermoplastic wax is added to the compound bulb & the patient goes through the same motions of moving the head down & from side to side.
- The child is allowed to converse with his parents so that the bulb becomes refined by muscle trimming through use.
- After this, the appliance is removed & the compound bulb is converted to acrylic.
- Any modifications if required are done similarly in the subsequent visits.
Meatal obturator
First described by Schalit in 1946, Advocated by sharry in 1955.
A meatal obturator establishes closure with nasal structures at a level posterior & superior to the posterior terminus of the hard palate
Closure is established with nonmovable tissues which include the turbinates, residual vomer & the roof of the nasal cavity.
Indicated for patients with extensive defects of soft palate who exhibit a very active gag reflex.
According to Desjardins (1978) it is the obturator of choice when retention is a problem. Since the meatal portion is closer to the palatal portion, less torque is produced.
Disadvantages
It does not allow the patient to control nasal air emission because it is placed in an area devoid of muscle function. Nasal airflow is created by drilling holes in the obturator or by reducing its lateral extensions.
There is distortion in nasal resonance as the oral cavity & oropharynx are increased in size and the nasopharynx is decreased in size.
Palatal Lift Prosthesis
First advocated by Gibbons & Bloomer in 1958.
Useful for patients with palatopharyngeal incompetence who exhibit compromised motor skills of the soft palate & the related musculature as in myasthenia gravis, cerebral palsies, & cleft palate patients.
Objective of a palatal lift prosthesis is to displace the soft palate at the level of the normal palatal elevation enabling closure of pharyngeal wall action.
If the length of the soft palate is insufficient to effect closure after maximal displacement, the addition of an obturator may be necessary behind the displaced soft palate
Hard Palate Obturator
Used when a perforation exists in the hard palate & the surgeon desires more growth of the child before surgical closure.
Speech bulb is not indicated as the soft palate has been repaired & is functioning well.
Impression is recorded, cast poured & a plate is fabricated.
Anterior Prosthesis
Between ages 9-14, due to lack of growth of the maxilla, there is pseudo mandibular prognathism.
At this time the prosthodontist can construct an anterior prosthesis which will restore function & create a pleasing profile.
Prosthetic Speech Appliances for Adults
- Removable prosthesis
- Fixed prosthesis
Removable Prosthesis
Preferred when there is a large anterior ridge defect and/or the middle third of the face is depressed.
They can be categorized as
- Snap on type
- Non snap on type
Snap on Prosthesis with No Speech Bulb
In cases of ‘V’ shaped ridge defect, poorly positioned & poorly shaped teeth are removed.
Abutments are prepared for full-coverage crowns (anatomically carved/ thimble) & a baker or a Dolder bar is used to splinting one side with the other.
An RPD is fabricated with a gold framework that overlays the bicuspids & clasps the molars. The clip attachment engages the anterior cross arch bar.
Removable Partial Prosthesis with No Speech Bulb
With large ridge defects & extremely poor occlusion, more teeth may be salvaged to increase the retention & stability of the superimposed denture.
This prosthesis restores the vertical, facial, & occlusal dimensions of the maxillofacial deformity.
Complete Superimposed Denture with No Speech Bulb
Full gold crowns placed on all maxillary teeth with precision gold framework & clasps for retention & stability of the overlay denture.
Overlay denture restores the vertical dimension of face & gives an ideal arch form to the maxillary arch with a full complement of teeth.
Snap on prosthesis with speech bulb
Similar to a child’s pharyngeal obturator except that the retentive clasps, and Velar & pharyngeal portions are fabricated in precise gold castings.
Crowning & splinting of existing teeth may be necessary prior to construct the speech prosthesis.
This appliance snaps to the bar, overlays the bicuspids, which are out of occlusion and brings the anterior teeth forward to help correct the middle face concavity.
Conventional speech prosthesis with bulb
In patients with a full complement of teeth & velar insufficiency, a framework clasping the healthy abutment teeth which carry the palatal, velar & pharyngeal portions is fabricated to improve the speech.
It is similar to the earlier one described except that it has a speech bulb & is to be used in patients with velar insufficiency so as to improve speech
Fixed Prosthesis
Preferable in cases where stability, longevity, comfort & hygiene can be accomplished.
A separate removable framework is necessary to carry the bulb into the pharyngeal area.
Resin composite restorations & porcelain veneers may be used to improve the appearance of teeth that need recontouring.
Kantarowicz in 1975 advocated extensive fixed bridgework involving several teeth on either side of the cleft.
Ramstad in 1973 & Johanson in 1974 advocated less extensive crown & bridgework with one or two abutments on either side of the cleft.
Currently, conventional principles of bridgework design are employed with avoidance of fixed restorations across the cleft where possible.
Renuka Emani
11 Jul 2020Wonderful notes !! Thank you ?
ปั้มไลค์
23 Jul 2020Like!! Really appreciate you sharing this blog post.Really thank you! Keep writing.
Anjali saini
12 Sep 2020Mam today when I study and watch your YouTube channel I found something for about dentistry knowledge THANK YOU SO MUCH MAM TO CONNECTING ME MORE TOWARDS MY PASSION…..
THANK YOU ???♀️
hey
12 Dec 2020Willie G youllied
What’s up to every one, it’s actually a good for me to
pay a quick visit this web site, it consists of priceless Information.
Pooja
19 Aug 2021Thanku so much but is there any video also for cleft lip and palate