TOOTH SUPPORTED OVERDENTURE
INTRODUCTION
It is considered that the presence of a tooth with a healthy periodontal ligament keeps a proper alveolar ridge morphology. In contrast, a diseased and / or absence of periodontal ligament is associated with certain residual ridge resorption. Because of this, contrary to the past where extractions of remaining teeth with complete denture replacement used to be promoted as an inexpensive and permanent solution for oral health care, nowadays, dentists try hard to maintain even loose teeth with bone loss to stabilize, retain and support the removable dentures.
A tooth-supported overdenture may be defined as a removable prosthesis that covers and is partially supported by natural teeth or natural tooth roots.
Overdentures are otherwise known as Biologic dentures, Hybrid dentures, Telescopic dentures, Overlay dentures, Superimposed dentures.
Overdenture therapy is actually a complete rehabilitation drawing upon many phases of dentistry i.e. Oral surgery, Periodontics, Endodontics, and Prosthodontics.
When an overdenture treatment is the method selected it does not simply involve making a denture to fit over the roots. The success or failure of many overdentures depends on detailed differences in design or fabrication. Failure to select the right abutment for each situation adds to the complexity of the treatment.
HISTORY
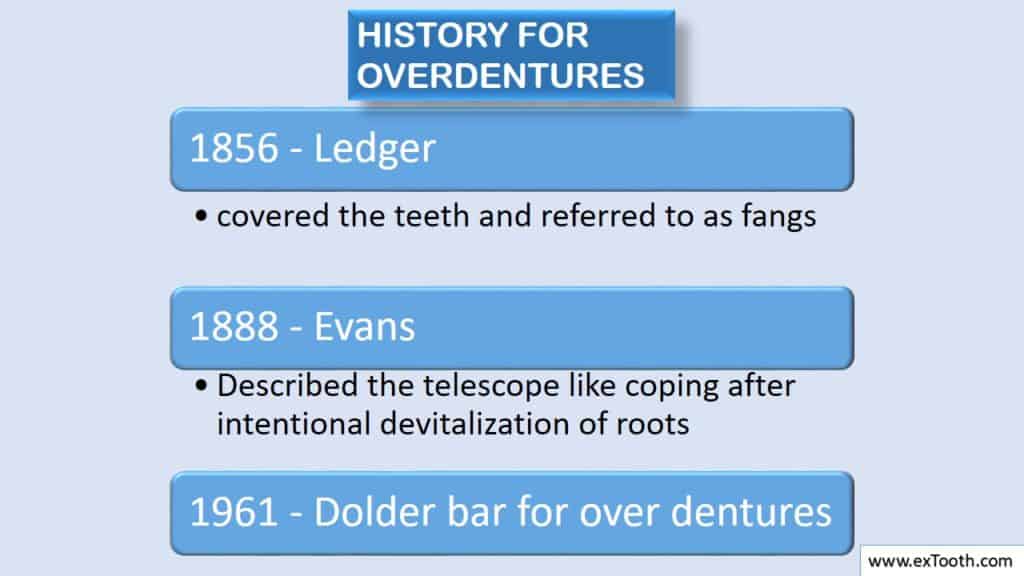
In 1856 Ledger constructed plates that covered the teeth and he referred the teeth to as fangs.
In 1888 Evans reported a means of using roots to preserve restorations.
In 1896 Essig described the telescope like coping after intentional devitalization of roots.
Dolder in 1961 introduced Dolder bar for over dentures.
RATIONALE
- TO INCREASE PATIENTS MANIPULATIVE SKILLS IN HANDLING THE DENTURE:
The function of the masticatory system depends on the sensory input placed into the system by various components like periodontal ligament, Salivary glands, epithelial surface of oral cavity, muscles of tongue, muscles of mastication and TMJ.
A defect or non-integration of the proprioceptive input can result in poor function or pathologic changes in the system.
Input from periodontal receptors forms a major part of inputs. They contain information about the magnitude and direction of occlusal forces, size, and consistency of food bolus. It also monitors teeth against overloading.
By preserving teeth, PDL is preserved, thus proprioceptive impulses are preserved.
Proprioceptive feedback in Overdenture patients is viewed as very close to that of edentulous individuals. This will help the patient in easy denture coordination and the ability to control the denture in his physiologic environment.
Jerge and Kawamura (J. Physiology 1964, 1967), suggested that periodontal receptors are actively involved in cyclic jaw movements during mastication. They suggested that the activity of specific muscles or parts of muscles attached to the mandible is directed by receptors of teeth.
Kapur and Collister (1970) presumed that the periodontal receptors acted a significant indirect role in the masticatory reflex by adapting the scale and nature of masticatory stroke.
Rissin et al (JPD 1978;39;508-511) compared masticatory performance in patients with Complete dentures and Overdentures and found that Overdenture patients have chewing efficiency one third higher than the Complete denture patients.
- TO DECREASE ALVEOLAR BONE RESORPTION:
One of the reasons why alveolar bone resorption occurs under conventional dentures is that all load is on mucosa. Mucosal receptors under conventional dentures are unable to discriminate the amount of load during mastication and consequently are unable to warn against occlusal overloading. With natural teeth, the proprioceptive input from PDL receptors is so discrete that excessive occlusal load signals the muscles to stop contractions.
(Threshold for load detection for denture wearers was >100 times than for anterior natural teeth.).
Crum and Rooney (JPD 1978; 40; 610-613) in a 5-year study found that the retention of mandibular canines for Overdentures led to the preservation of alveolar bone. They found that there is 8 times less bone loss in patients with Overdentures. They observed that the use of Overdentures preserved the alveolar bone between canines (in both height and width). Overdenture patients also exhibit a less alveolar bone loss in areas immediately posterior to canines.
TO RETAIN THE TEETH AS A PART OF ALVEOLAR BONE:
Advantages are:
1) Better support
2)Better masticatory function
3)Increased retention by using attachments.
ADVANTAGES
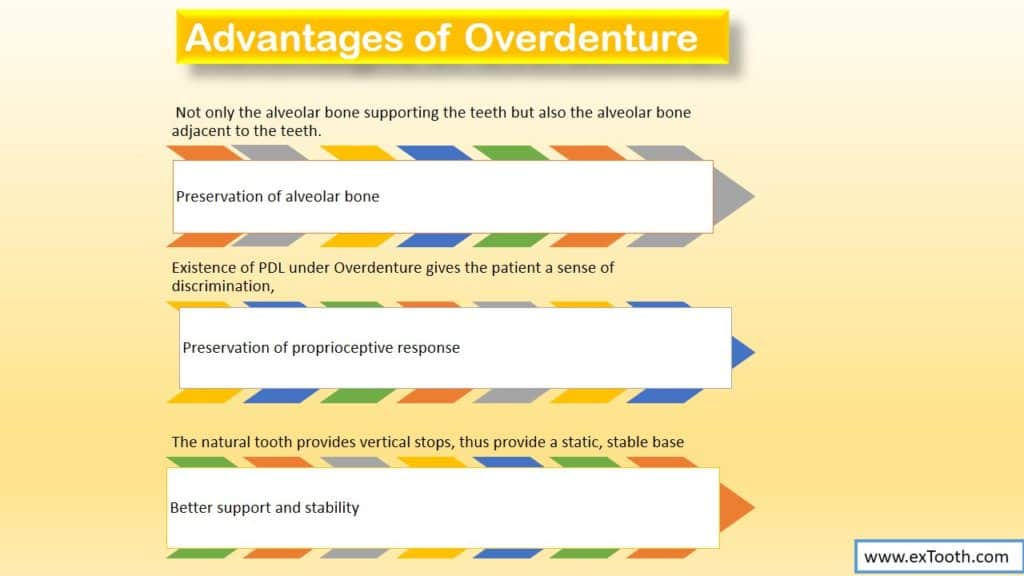
- Preservation of alveolar bone:
Preserving teeth retains not only the alveolar bone supporting the teeth but also the alveolar bone adjacent to the teeth. - Preservation of proprioceptive response:
Existence of PDL under Overdenture gives the patient a sense of discrimination, which is not possible with conventional dentures. - Better support and stability:
The natural tooth provides vertical stops, thus provide a static, stable base.
(Occlusal forces will be sustained by Periodontal Ligament. The area left by mucosa for support is 1/4th that of PDL that is present in a dentulous subject. This leads to greater efficiency and comfort if hygiene is good.)
Increased Retention:
Retention is usually sufficient merely by overlaying the teeth. When more retention is required attachments can be used.
- Patients acceptance:
Patients are more receptive and appreciative to this treatment because they experience a striking improvement in function and esthetics while still maintaining some of their own teeth.
(Thought of retaining at least the root structure or some coronal portion of the natural teeth is emotionally uplifting to many people). - A simple approach to problematic patient:
Patients with congenital defects like Cleft palate or defects arising from surgery or trauma are often difficult to treat because of difficulty in getting support and retention. Designing Overdentures with attachments can be a remedy in these situations. - Convertibility:
If some teeth are lost, denture can be readily converted to accept the alteration. Even if all the teeth are lost, Overdenture can be relined in conventional complete dentures. - Post insertion problems are minimal.
- Open palate is possible.
- Ideal occlusion-because of minimal Relief.
DISADVANTAGES
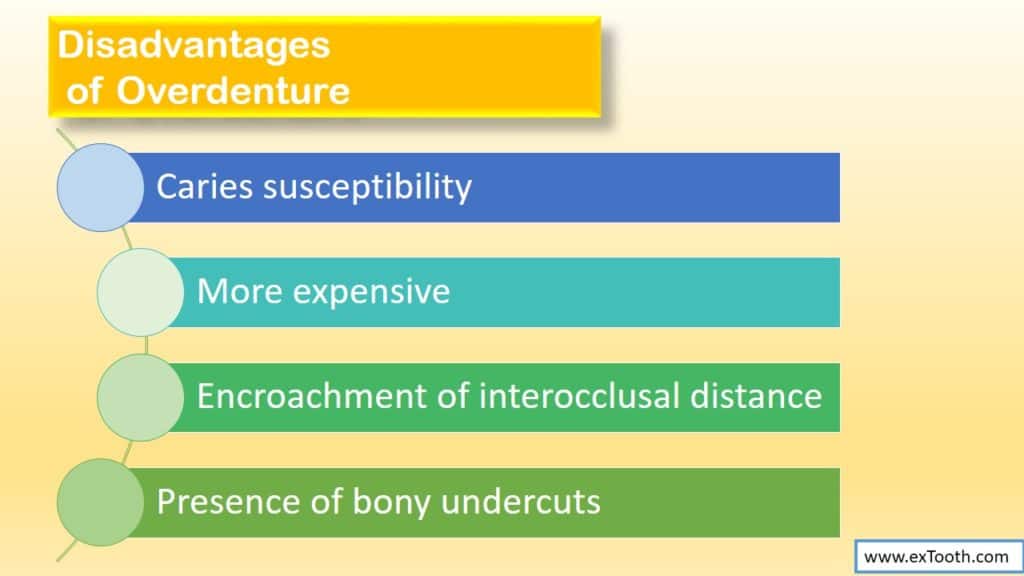
- Caries susceptibility:
Needs precise home care and fluoride applications. - More expensive:
More pricey than regular denture because of Endodontic treatment, periodontal treatment, and high-priced attachments. - Encroachment of interocclusal distance:
- Presence of bony undercuts:
Bony undercuts, particularly near the overlayed teeth, may create obstacles (in respect to the intimate adaptation of denture flange to underlying tissues.)
A) We can block out these undercuts and free that area: OVER CONTOURING
This creates a denture flange that is spaced away from the tissue. This can:
a) Create food trap.
b) Decreases retention, since peripheral seal is broken.
c) Over contouring, leads to a poorly contoured base resulting in improper lip fullness, which is difficult for patient to accept (poor esthetics).
Over contoured flange does not interact well with the facial musculature, thus decreasing the support and retention of denture.
B) We can purposely shorten the denture flange to end it at the height of contour: UNDER CONTOURING
There will be no peripheral seal, thus decreased retention, decreased stability, food entrapment and poor esthetics.
C) Surgical intervention:
It is usually not possible, since the bone involved is the supporting alveolar process of the overlaid tooth.
Freidline and Wical: described a technique to block out a bony labial undercut through the use of a free soft tissue palatal graft. Added benefit is increased zone of attached gingiva and apical positioning of soft tissue attachment.
- Fracture of denture base:
In several situations, due to a shortage of free space, parts of the Overdenture base are quite fragile and are likely to fracture.(Metal reinforcements may be used) - Bulkier than conventional FPD /RPD
INDICATIONS
- Patients with poor prognosis for conventional complete denture:
a) High palatal vault and ridge support:
(Difficult to make a stable retentive maxillary denture)
b) Knife edge ridge: provide inadequate support.
c) Inadequately explained sub lingual space and class III tongue position:
(Positive retention and stability are hard to achieve.
Class III tongue position: tongue is retracted and depressed into floor of the mouth with the tip curled upward or downward- unfavorable tongue position as it drops the level of the floor of mouth and does not provide an adequate lingual seal. If we extend the flange to gain the border seal-will result in an overextension during tongue movement and would dislodge the denture.
- Few natural teeth remaining which are badly tilted or are unsuitably shaped to provide abutments for normal partial denture.
- Prognosis of the remaining teeth poor: Over denture can serve as transitional denture prior to the loss of the teeth, Endodontic Treatment, crown root ratio decrease and stabilized.
- Severe generalized attrition cases.
- Complete denture opposed by natural dentition especially lower anterior teeth:-combination syndrome chances.
When a pronounced vertical overlap of the anterior teeth is required to produce a good esthetic result:-necessary to retain few maxillary teeth for overdenture.
CONTRAINDICATIONS
- Uncooperative and under-motivated patients:-who ask on the extraction of remaining teeth.
- Any patient who will not participate in oral hygiene and routine office procedures:-like recall appointments for adjustment, which are needed to maintain the remaining teeth and supporting tissue in a state of health.
- Mentally and physically handicapped patients:- difficult to maintain good oral hygiene .
- Patient can not afford treatment cost.
Inadequate inter-arch space: (adequate–16-18mm in premolar area).
PATIENT SELECTION
It is important for fabrication of successful Overdenture.
- Possibility of fixed or removable partial denture.:-
If remaining natural teeth are capable of supporting a fixed or removable partial denture, then this form of treatment must be considered primary plan of treatment.(4 or less – go for OD, not universal rule, full attrition – OD) - Caries status:-
Presence of high caries index and the creation of a situation that will easily promote a caries environment are two of the most devastating squeal of improper OD patient selection.(If abutment teeth are caries prone then seriously question this mode of treatment) - Patient age:-
Extractions to be avoided in young patients as far as possible, so
(Maintenance of teeth and supporting bone , should always be considered over-extraction in young patients. Because of the length of time OD will be in service, failure of the appliance will be there in long run. Individual tooth therapy and home care become more crucial) - Abutment selection:
During examination there are many factors to be considered in abutment selection like:
A) Periodontal status
B) Endodontic status
C) Caries status
D) Location and number of abutment
E) Space between abutments.
A) Periodontal status
Since Overdentures rely on abutment teeth for support and stability, hence these teeth must be in a balanced state of periodontal health before the completion of the Overdenture.
Teeth with a hopeless periodontal prognosis should not be picked as abutments. Prospective abutments should have:
i) Minimum mobility: Although mobility patterns are important in selecting abutments, improvement in crown, root ratio – decreases apparent clinical mobility significantly.
ii) Adequate bone support: At least 6mm of bone support is needed to retain a tooth as an Over Denture abutment.
iii) Should be amenable to any indicated periodontal treatment.:- Periodontal pockets, bony defects be eliminated before commencing treatment.
Common problem is lack of adequate attached gingiva.
Attached gingiva:-
1.teeth periodontally involved
2.supports marginal gingiva
3.allows deflection of food away from marginal gingiva
4.maintain oral hygiene.
Increases with age and with supra eruption.
Normal, maximum attached gingiva in Anterior Region
Maxilla: 3.5-4.5mm, mandible: 3.3-3.9mm
Least in first premolar area.
After overdenture (OD) is inserted, the functional forces of mastication and of the tongue are not applied to the gingival tissues. The reduction in functional stimulation can cause decrease in keratinization and make these tissues more susceptible to injury.
Attached gingiva can be created by mucogingival surgeries like partial thickness graft or apically repositioning split thickness flap.
Toolson and smith (JPD 1982:41;4-11 and JPD 1983:49:749-756), did a 2 year and 5 year study on OD patients.
2 year Study showed elevated plaque scores on abutment teeth but no significant decrease ion periodontal health. They emphasized the importance of adequate follow up and continued reinforcements of home care procedure.
5 year study showed that
a) Periodontal health was not at an optimum level. (Though still not responsible for loss of significant number of teeth.)
b) There was a loss of attached gingiva between second and fifth year follow up.
Contraindication for using periodontally involved teeth are:
i) Grade III mobility due to loss of alveolar bone can not be corrected.
ii) Failure to establish zone of attached gingiva by mucogingival surgeries.
iii) Osseous defect which can not be corrected by surgery.(can be alveolar bone of abutment so we may decrease the support of abutment.)
B) Endodontic status
Endodontic treatment is recommended for OD abutment as it allows enough reduction of the crowns (as directed by esthetics and vertical height requirement)
Ideally single rooted teeth and a single canal that can be easily negotiable are best candidates. (Although multi rooted teeth can also be used)
Vital teeth and even those having ample secondary dentine are not very acceptable abutments.
(Due to the fact that secondary dentine does not form an absolute seal, early radiographs are necessary if vital teeth are used as OD abutments.)
to decrease the cost of treatment we should consider the teeth that have already been treated endodontically. (Carefully evaluate – should not select wrong abutment).
C) Caries status of abutment
Ideally teeth with minimal caries or no varies involvement should be selected as abutments.
If caries present, evaluate if it can be easily removed and if we can create an environment that the patient can maintain. (An active caries process can lead to recurrence of caries in unprotected abutment teeth or gingival to coping margins, and thus can lead to failure of the OD).
D) Location and number of abutments
If patient presents with >4 retainable teeth in an arch that are periodontally sound: some other treatment modality (RPD, FPD) should be considered first. (Exception based on individual cases and pt. desires).
Location of teeth is important for support of OD and preservation of the alveolar bone.
Anterior aspect of residual ridge, especially that of mandibular is very susceptible to change therefore canines and premolars are valuable teeth to preserve in this area.
Preservation of upper anterior teeth is especially important if denture opposes natural teeth in the anterior mandible. (Combination syndrome prevention, Prevent destruction of anterior maxillary ridge).
If 4 abutments in one arch i.e. 2 canines and 2 second premolars – represent an ideal stress distribution. This distribution provides maximum stability and support for the OD which is truly tooth supported.
Another favorable arrangement-use of maxillary canines and a central incisor – provides a tripod of support in the anterior jaw ; particularly effective when opposing natural dentition.
If 3 abutments – 2 on one side of the arch – can cause unbalance (generally patient had no difficulty)
If only 2 abutment teeth (Most commonly seen condition)
Should be situated bilaterally for optimum support
2 canines, a canine, and a premolar, or 2 premolars are desirable and preferred to 2 molars. (Since the anterior position of canines minimizes the soft tissue loading in the anterior arch.)
Canines > premolars > incisors > molars
Canines are used most commonly as abutments (up to 80%) (Since can be easily endodontically treated, have adequate periodontal attachment, least caries susceptible, strategic position).
E) Space between abutments
Results are better if abutments are not approximating because:
- They do not provide more support and stability than 1 abutment. (i.e. 1 canine and 1 premolar =canine (in regard to support)).
- More difficult for patient to keep abutments clean.
- May make tooth positioning on OD more difficult.
- Connectors have to be cleared up from the gingiva which can hinder lab procedures.
TYPES OF OVER DENTURES
Depending primarily on the status of the patient’s dentition at the start of treatment. (According to Brewer):
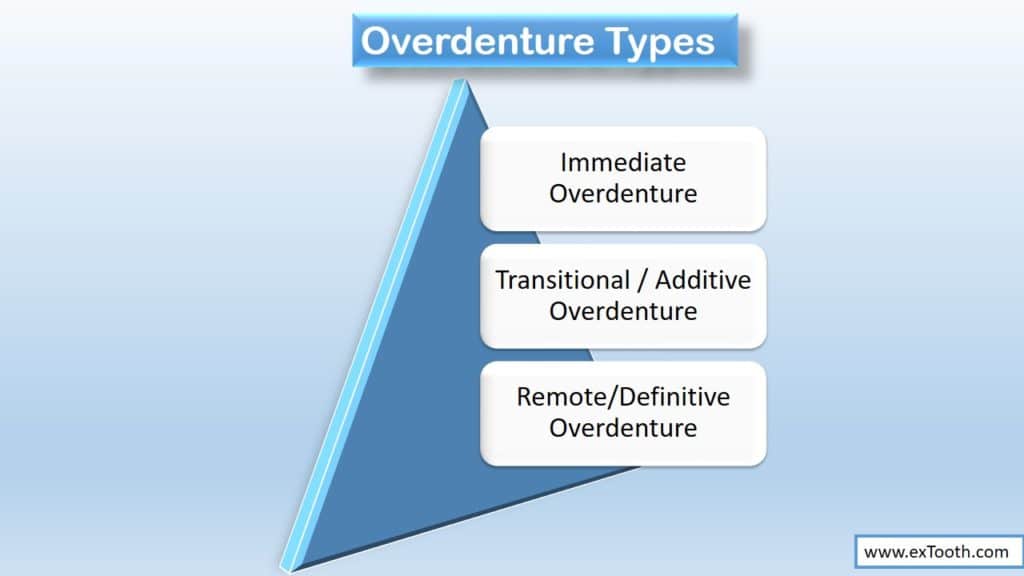
- Immediate OD
- Transitional / Additive OD
- Remote/Definitive OD
Immediate Overdenture
An immediate overdenture is constructed for insertion immediately after the removal of some natural teeth. The remaining natural teeth are treated and the overdenture is inserted as an immediate replacement.
Construction of a definitive overdenture requires special attachments or castings over restored abutments. These procedures are more time consuming and costly.
An immediate overdenture is easy to use and uses no specialized castings. So it can be used as an interim prosthesis that allows the dentist, opportunity to evaluate the response of the abutments and supporting tissues to an overdenture and to observe the oral hygiene.
It is reliable prognostic aid and a pre requisite to the more sophisticated technique.
If response is poor and failure of abutments is sure;the immediate overdenture can be converted to conventional complete denture.
PROCEDURE
Like Immediate complete denture.
Select the teeth to be retained as abutments.
If arch has large number of hopeless teeth, remove posterior hopeless teeth in increments (like immediate complete denture.), (one side at a time), (6 wks healing time).
(When proposed immediate overdenture is opposed by a natural dentition or by another overdenture, pre treatment measurements between selected points are recorded.(acts as guide in reestablishing VDO)).(Premolars retained to act as vertical stops).
Hopeless anterior teeth retained for esthetics and function considerations until insertion of immediate overdenture.
During healing period – Endodontic and periodontal treatment of proposed abutments is done. (Endodontic treatment of all abutments, periodontal treatment to correct pocket depths, to recontour supporting tissues.)
Oral hygiene procedures are emphasized.
After healing
Dual impression of the arch is taken:
Custom tray for edentulous area- border molding- impression with ZOE/rubber base- use alginate –dual impression-poured in dental stone.
Adapt base plate –make occlusion rims-record jaw relations (centric jaw relation)
SELECTING AND POSITIONING TEETH (method by Lord and Teel, DCNA 1969;13;871-881):
Denture teeth of appropriate mould and shade selected
Positioned by removing one tooth on the cast and substituting the corresponding replacement.
All teeth except those serving as abutments are replaced by denture teeth.
Abutment teeth on the cast are prepared.
Each abutment tooth shortened to a height of 3-4mm and the axial surfaces are tapered to remove undercuts and create space for the denture tooth replacement. (Reduction should be sufficient to make resin thick enough (at least 2mm) to avoid fracture of base.).
Reduction of abutment on the cast should be less than anticipated for natural tooth.(which is prepared at the time of insertion).-to allow placement of overdenture without interference.
Abutment height is measured on the cast and used as guide during preparation of abutment for patient.
Resin denture teeth selected before preparation.
Hollowed with no.8 bur.
Denture waxed and flasked in conventional manner – dewaxed – packed with heat cure denture base resin – recovered – trimmed and polished.
Margin around each abutment indentation is smoothened to minimize gingival irritation.
Overdenture ready.
Recall patient –abutment teeth prepared immediately before removal; of last hopeless teeth.
Abutment teeth reduced in a manner similar to that used on the cast.(but should be small –to allow placement of overdenture without interference.)
Abutment teeth should be 2-3mm high and axial surfaces tapered .Abutment surfaces are smoothened. Amalgam/composite restoration placed on occlusal surface to seal root canal.
Prepared teeth treated with APF gel (1.23%F) for 1 min-2 applications.
Remove hopeless remaining anterior teeth (remove as atraumatically as possible)
Overdenture is inserted – occlusion is checked – patient instructed not to remove until first post operative visit (on next day).
Overdenture cleaned-corrections made
Interferences if present between overdenture and abutments are removed (using Kerr disclosing wax).
Adaptation of overdenture to the abutment with autopolymerising resin done on first post insertion appointment.
Polish abutment teeth. (Rubber cup and flour of pumice).
Overdenture is adapted to the abutment teeth by adding tooth colored autopolymerising resin to the abutment indentations of the denture.
Small hole is placed in the depths of the indentation to vent the excess resin.
Abutment tooth lubricated with petroleum jelly (to prevent sticking of acrylic)
Tooth colored acrylic resin placed into indentation.
Overdenture inserted-removed before complete hardening-excess removed (to minimize gingival irritation).
Oral hygiene instructions given to patient (use soft bristle brush, dental floss, clean after each meal).
RELINING- same like conventional relining. Generally necessary to maintain adequate tissue adaptation.
If response is poor and oral hygiene inadequate:
Better avoid initiating more definitive prosthesis. Continue-try increase patient motivation
If abutment failure is sure:
Overdenture can be converted to conventional complete denture by relining after loss of abutment.
If response is good:
(1.minimum crevicular depth, 2.absence of plaque on abutment, 3.minimum mobility of abutment, 4.excellent tissue color and tone):
More sophisticated overdenture can be considered.
Transitional / Additive Overdenture
A transitional overdenture is obtained by converting an existing RPD to overdenture.
Considered as temporary or interim overdenture.
ADVANTAGE
- Less costly compared to conventional overdenture.
- The patient’s previous experience with the partial denture permits a smooth transition to overdenture status.
DISADVANTAGE
Old RPDs might have-
- Inadequate occlusion
- Inadequate border extension
- Inadequate support and stability.
Therefore may make satisfactory conversion difficult.
CONVERSION
Canine and premolar remaining
Endodontic treatment of abutment teeth done-alginate impression is made of the arch with partial denture in place.
Impression placed in humidor (to prevent unnecessary drying and dimensional change during abutment preparation)
Abutment teeth prepared
Autopolymerising resin of proper shade placed into the abutment indentation of alginate impression.
Impression with partial denture seated in mouth – removed before complete polymerization.
Stone cast poured into impression with partial denture in place (Vaseline to partial denture).
( In numerous hopeless teeth remain, conversion can require several intermediate modifications. Therefore resin denture teeth are added to the partial denture before the hopeless teeth are removed. The partial denture functions as an immediate prosthesis that can be converted to transitional overdenture after healing and Endodontic treatment.).
Flanges added with autopolymerising resin-trimmed, polished.
Inserted in mouth and occlusion checked.
Usually Transitional overdenture is replaced by more definitive overdenture after 8 months to a year.
If response is good – go fro Remote overdenture.
If this is working good – can put copings on abutments and modify this according to copings.
Remote/Definitive Overdenture
This is an overdenture other than Transitional or immediate overdenture.
It is usually built for insertion at the time ‘remote’ from the extraction of dying natural teeth.
TREATMENT PLANNING
Overdenture Patient
Prerequisite Oral Surgery
Prerequisite Periodontics
Prerequisite Endodontics
Immediate Overdenture
Convert To Conventional Complete Denture
Continue Immediate Overdenture
Remote Overdenture
Exam. Diagnosis, Treatment Planning, Oral
Hygiene Counselling
Remove Hopeless Teeth, Oral Hygiene Counselling
Abutment Supportive Treatment, Oral Hygiene
Counselling
Abutment Endodontic Treatment
Oral Hygiene Counselling
Poor Oral Hygiene, Imminent Abutment Failure
Marginal Oral Hygiene And Overdenture Response
Excellent Oral Hygiene And Response To Immediate
Overdenture
Copings, Metal Base Or Attachment Overdenture.
Continue Immediate Overdenture
CLASSIFICATIONS
A) Based on the method of abutment preparation (Heartwell)
- Non-coping with simple tooth modification (a)With Endodontic treatment
(b) Without Endodontic treatment - Coping
(a) Short coping
(b) Long coping - Attachments
- Submerged vital roots
B)Prieskel classification of overdenture
- Transitional overdenture
- Immediate overdenture
- Remote / definitive overdenture
- NON-COPING
A)WITH ENDODONTIC TREATMENT:
- Widely used.
- It is indicated when no enough space present for OD; so teeth have to be drastically reduced.
- Caries index should be low
- Excellent home care is needed.
After Endodontic treatment, abutments are reduced to a coronal height of 2-3mm and then contoured to convex or dome shaped surface. Amalgam or composite restoration is placed into the exposed root canal.
Remaining dentine smoothened and polished, leaving surface that accumulates minimum plaque and can be easily cleaned.
B)NON-COPING WITHOUT ENDODONTIC TREATMENT:
Remaining teeth are merely reshaped to eliminate undercuts and reduce vertical height (if necessary) to create more inter ridge space for the OD.
- Caries index should be low
- Good oral hygiene is needed.
If teeth are reduced to any degree, the vital pulp must be receded sufficiently so that reduced teeth are not sensitive (severe attrition).
Used in partially anodontic patients or in patients with severe attrition.
Minimal preparation which makes the procedure totally reversible.
- COPING:
Cast metal coping with a dome-shaped surface and chamfer finish line at the gingival margin (or slightly supra gingival) are fabricated and cemented.
2 types of copings:
a) Short copings
b) Long coping
a) Short copings:
2-3mm long and normally require Endodontic treatment (because the required coronal tooth reduction would expose the pulp).
Attached to the casting is a post fitting to the canals.
Dome shaped:-Abutment is reduced in height and width (i.e. circumference)
Chamfer finish line.
b) Long coping:
5-8 mm long
An attempt is made to avoid Endodontic treatment by conservative reduction of coronal tooth structure (but generally endodontic treatment recommended to avoid later failure)
Long ellipsoid shaped-minimal height reduction, taper-2-6 degrees
Larger crown root ratio, therefore, require greater level of osseous support.
Adequate inter occlusal distance should exist. - ABUTMENTS WITH ATTACHMENTS:
Objective of attachment is to improve retention of the denture base.
The attachment does not reduce the crown-root ratio significantly as does the cast coping, so abutment need adequate bone support because of added stress.
Because of stresses on the attachment from the OD, more retention is needed in the casting. This is done by using post (post and core).
Since, the attachment usually requires some form of the inter ridge distance, sufficient space is necessary for its construction.
Because of added time, cost and risks the procedures should be reserved for patients with favorable prognosis.
Occlusal surface is similar to dome shaped coping but the centre of occlusal surface is hollowed out to increase the strength of the dowel/ diaphragm junction and also to decrease the space requirements of the attachments.
Anti-rotation slot is important and the length of dowel in the canal needs to be at least 10mm.
OVERDENTURE ATTACHMENTS
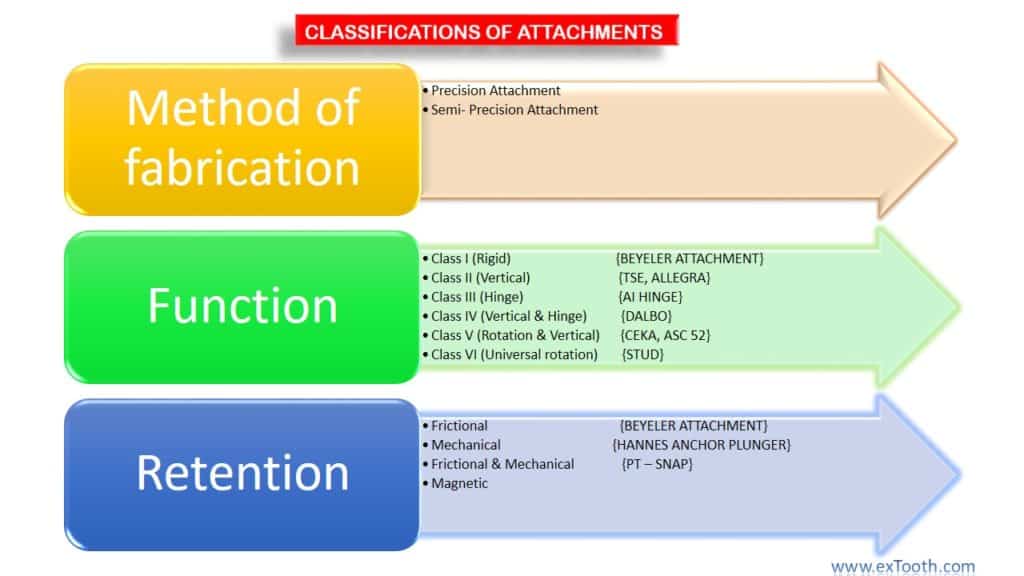
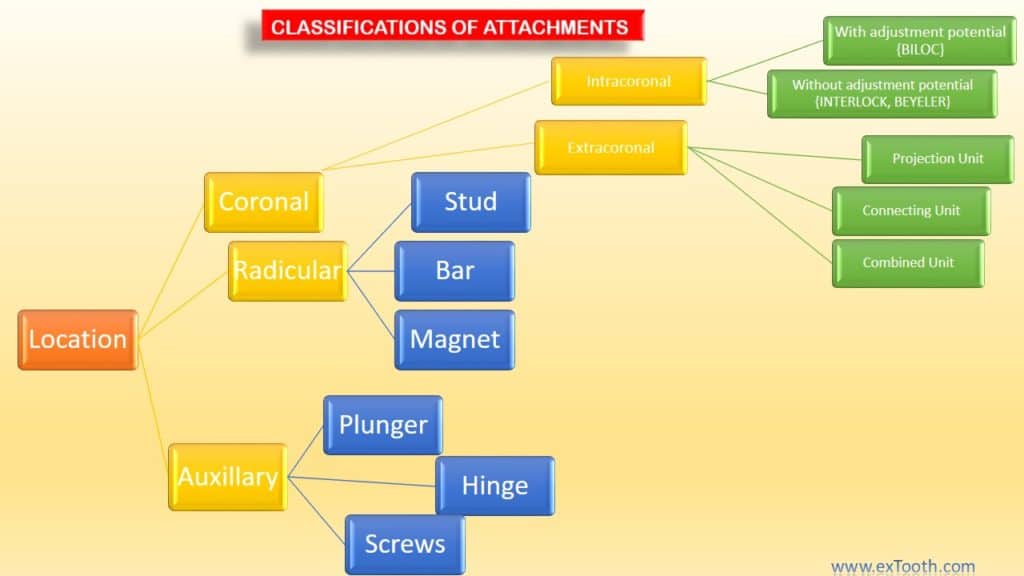
OVER DENTURE ATTACHMENTS CAN BE CLASSIFIED AS:
- Intra radicular attachments. Eg: zest anchor
- Extra radicular attachments. a) Stud attachments. Eg: Rothermann, Dalbo, Bonaball b) Bar attachment. Eg: Dolder bar, Hader bar, Ackerman clip
- Magnet attachments.
Intra radicular attachments

Example-Zest anchor
-Derives its retention from with in the root.
-Post preparation is made with in the rest and a Female sleeve (Stainless steel) is cemented into the root.
-Female portion is a nylon post and a ball head
-Female portion is attached to the Over Denture as a chairside procedure.
(Post is placed in a recess to accept this female part. Nylon post is placed in the sleeve and is picked up in the denture resin).
-Retention gained by ball head snapping into the undercut in the female sleeve.
Advantage:
- Space problem is less since attachment is inside the root.
- Minimal leverage on the abutment tooth since the point of attachment is below the alveolar bone level.
- Attachment used without a dowel or coping.
- Pickup in the denture with resin is easy
- If more than one tooth is used parallelism of attachment is not necessary because of the flexibility of the nylon male part.
- Provides slight vertical and rotational movements.
- Can be used on divergent teeth.
- Simple to use and inexpensive.
Disadvantages:
- No coping – root exposed-susceptible to caries – meticulous oral hygiene needed.
- Nylon male portion absorbs waterà – prevents entry of the attachment.
- Nylon male portion bends and breaks very easily; it can require replacement as frequently as every 2-4 months.
- When many Zest anchors are used in mouth male nylon portion may bend preventing proper seating.
- If the patient attempts eating without denture-food enters female housing which is very difficult to remove.
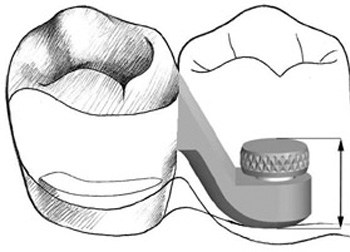
Extra radicular Stud attachments

Most stud type attachments consist of a male Stud type that is soldered to the base
Base is a coping covering the prepared root stump usually having a post extending into the treated root canal.
Fixation is attained by a female housing which is embedded in the acrylic of the OD.
Stud attachments can be:
- Resilient studs
- Non Resilient studs
RESILIENT STUDS
Examples:
Resilient Gerber
Resilient Ceka
Resilient Rothermann
Bonnaball
Resilient Bonna cylinder
Resilient Dalbo
Ancrofix
-Allow some movement of the denture base.
-Can be unidirectional or multidirectional.
-Used when there is an inability to develop a well fitting denture base.
NON – RESILIENT STUDS
Examples:
Non- Resilient Gerber
Non-Resilient Ceka
Non-Resilient Rothermann
Introfix
Non-Resilient Bonna cylinder
Non-Resilient Dalbo
Do not allow movement of Overdenture.
GERBER ATTACHMENT (European)

2 TYPES:
A) Non resilient /Gerber cylinder.
B) Resilient.(Allows vertical movement of base).
A) NON RESILIENT GERBER
- Most commonly used.
Consist of 5 parts
- Soldering base- Male part
- Male post- Male part
- Retention ring- Female part
- Retention spring clip- Female part
- Tent shaped housing- Female part
- Overall height is 4mm.
- Housing is available in 18/8 Stainless steel
- Male post and solder base are of a special high fusing alloy.
Advantage:
All components are replaceable and solder base is interchangeable with resilient Gerber,and with schubiger system also.
- Solid fixation and minimal torque on the tooth if the denture base is adapted adequately.
- Fabrication is simple.
- Provides adequate retention.
- Despite some disadvantage it is highly recommended.
Disadvantage:
1) Expensive.
2) Attachment can place torque on the tooth if denture base is not adapted adequately.
3) Mandrel is required to parallel the attachments when more than one
attachment is used.
B) RESILIENT GERBER
- Spring-loaded vertically loaded resilient attachment.
- Also known as Puffer.
- Consist of 9 parts.
- Overall height is 4.7 mm.(recommended when inter arch space is adequate)
- One of the most sophisticated stud attachments.
- Most expensive stud attachment.
- Imparts less torque on abutment – allows denture to utilize more of the residual ridge for support.
ADVANTAGE
1) All components are replaceable and interchangeable solder base.
2) Spring loaded resiliency allows the base to adapt under function.
3) Resilient attachment can be made non resilient by keeping a copper shim (0.4mm thick) in the female housing.
DISADVANTAGE
- Bulky:-Takes up the replacement tooth space.
- More complex:-Requires more skill.
- Resilient spring needs to be changed every 4 months.
- Mandrel required for paralleling if more than one attachment is used.
- Expensive tool kit is required for servicing the unit.
QUINLIVAN ATTACHMENT (Snapper-Quinlivan-1973)
This attachment consists of a prefabricated resin ball that is incorporated with the wax-up of the post and coping.
Completed casting is cemented into the endodontically treated tooth.
Dome shaped resin Female housing is attached to OD with Cold cure resin.
Retention is gained by an O rubber ring inside the housing.
This rubber ring is secured by a small lip in the orifice of Female cap.
This attachment allows rotational movement and gives minimum torque to the tooth.
ADVANTAGES
- Overall height is 3mm-can be used in limited space areas.
- Can be used in divergent abutments.
- Provides good retention.
- Easy to use.
- Provides fixation with rotational movement.
- ‘O’ ring can be easily changed.
DISADVANTAGES
- Male component, which is cast, could have porosities.
- Wear of male portion.
(Commercially available-OSO)

3 TYPES:
- RIGID
- RESILIENT
- STRESS BROKEN.
All are composed of male unit that is attached to the tooth and a female housing imbedded in the denture base. - RIGID DALBO
Has a cylindrical male unit with a round head that is attached to the tooth and a female housing imbedded in denture. - RESILIENT DALBO
Sphere shaped male unit which allow rotational and vertical movement ( made possible because of a relieved space between the units) of the female unit around it.
- Smallest and most commonly used.
- STRESS BROKEN DALBO
Similar in design to resilient type but female housing is longer and incorporates a coil spring.
Retention of all three types is provided by some what retentive arms of the Female unit fitting over the undercut head of the male unit.
2 TYPES:
A) RIGID TYPE
B) RESILIENT TYPE
Solder base with removable metal stud.
Male part is conical in shape and has a rounded top with increased diameter for retention.
Male portion is quartered vertically into 4 flexible sections to engage undersized female housing.
In resilient Ceka –space between female and male part-provides vertical and rotational movement.
Overall height is 4.1 mm-Resilient and 3.65 mm Non Resilient/Rigid.
ADVANTAGES
1) Allow for either rigid or resilient fixation.
2) Lamellae are adjustable and male stud is removable.
3) Servicing is easy.
DISADVANTAGES
- More height and bulk.
- Non resilient Ceka can produce excessive torque on the teeth unless overdenture base is adapted correctly on residual ridge.
Resilient Ceka in OD – When inter-occlusal space is sufficient and when vertical and rotational movement is desired.
Overall height of Ceka is misleading because screw base which is 1.4mm becomes a part of coping, therefore decrease the overall height by 1 mm.
BONA BALL ANCHOR
Solder base with a sphere.
An adjustable housing for 4 asymmetrical spring lamellae- that provides retention.
Lamellae surrounded by PVC rings to assure their action.
Overall height – 4mm.
Studies by Dolla-Bona- 1962, showed that after 50,000 insertions the retention was decreased by 20%. This diminished retention can be restored by bending the lamellae.
ADVANTAGES
- Easy to use.
- Lamellae can provide retention adjustments and compensate for wear of the metal ball.
(Recommended for OD when rotation, resistance and fixation are desired.)
DISADVANTAGES
- Male component is not replaceable.
- A mandrel is required for paralleling two or more attachments.
BONA CYLINDER ANCHOR
2 TYPES:
A) RESILIENT TYPE
B) NON RESILIENT TYPE
- Similar in design to Bonaball anchor.
Male post is cylindrical, has dome shaped head and is attached to solder base.
Number of asymmetrical lamellae increased to 8 to provide softer and precise retention.
A PVC ring surrounds the lamellae.
Overall height is 3.3 mm.
When spacer ring is usedà Bona Cylinder changed to resilient cylinder .Height-3.7mm.
ADVANTAGES
- Increased number of lamellae provides softer and more precise retention.
- If 1 or 2 lamellae break retention in the housing is still adequate
- Easy to use.
DISADVANTAGES
- Male component is not replaceable.
- Mandrel is required for paralleling when 2 or more attachments are used.
- Cylinder configuration can produce some torque on the tooth if the denture base is not adapted adequately.
One of the smallest and most popular Stud attachment.
Recommended for OD when occlusal space is limited or when only solid fixation or fixation with tissue or vertical resilience is needed.

- Most popular attachment.
- Short stud attachment.
2 types :
a) Resilient type
b) Non resilient type
ROTHERMANN NON RESILIENT
2 parts:
- Male stud with a solid core for (free hand) soldering.
- Female clip- consisting of perforated retention beam with split c ring extension.
Usual orientation is retention bar lingual to tooth.
Over all height- 1.2mm.
Can be used any where in mouth. Generally used in canine and premolar region.
ADVANTAGES
1) Attachment low in height-shortest extra coronal attachment.
2) Less lab time- Due to free hand soldering.
3) Retention can be adjusted by spreading the retention ring.
4) Torque is minimal.
5) No parallelometer is required and attachment can be aligned on divergent teeth as much as 10 degree from long axis.
(Female part attached to the denture base with cold cure acrylic)
(Only orientation required is the notch on stud, face opening of C-ring.)
DISADVANTAGES
1) Lingual bulk present.
2) No path in or guidance for seating the denture.-so patient finds it difficult in properly placing the appliance .Lack of a path and lack of thickness of acrylic due to lingual bulk leads to fracture of denture.
ROTHERMANN RESILIENT
Overall height of male stud is increased. i.e. 1.7mm.
Attachment allows some vertical and rotational movement.
Recommended when space is limited, teeth are divergent and vertical as well as rotational movement is desired in addition to fixation.
INTROFIX ATTACHMENT
Solid cylinder attachment.
Consist of three parts
- A solder base with threads.
- A replaceable and adjustable male part.
- Female cylindrical housing.
Male post is split longitudinally to allow adjustment of retention.
Available in two heights, 4.7mm and 6mm.
Can be used for fixed removable bridge as well as for OD.
ADVANTAGES
1) Simple to use.
2) Components are replaceable.
3) Attachments provide good seating and retention.
4) Ideal for ODs with Quadrilateral support.
DISADVANTAGE
1) Require mandrel for paralleling.
2) Torque potential maximum if denture base is not adapted adequately.
ANCROFIX ATTACHMENT
Resilient pressure button system.
4 parts
- A solder base
- A replaceable retention head
- A housing with 4 lamellae that can be activated
- A Teflon ring to allow lamellae to function in the resin.
-Height-3.2mm.
ADVANTAGES
1) Allows rotational movements.
2) Components can be replaced.
3) Retention can be easily adjusted.
4) Solder base is interchangeable with the Introfix attachment.
5) Simple.
DISADVANTAGES
1) Paralleling mandrel required if greater than 1 attachment is used.
2) Can place torque on teeth.
Some other attachments are: Baer F.G.Attachment, Biaggi Attachment.
BAR ATTACHMENT

Divided into 2 groups
A) BAR UNIT B) BAR JOINT
Bar unit provides rigid fixation for the OD, whereas bar joints permit some degree of rotational or resilient movement or both.
Primary function of bars are splinting the tooth and carrying appliance positionally.
When we select a bar it is desirable to select the largest possible size for space without affecting the vertical relationship, occlusion or contour of the prosthesis.
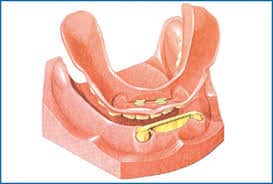
DOLDER BAR

A) DOLDER BAR UNIT
B) DOLDER BAR JOINT
DOLDER BAR UNIT

- Has ‘CHURCH WINDOW PROFILE’ i.e. rounded top and parallel walls.
- To this fits the rider clip-which is embedded in the acrylic.
- Retention is by friction fit
- Rigid fixation
B) DOLDER BAR JOINT - Same as Dolder bar unit, except shape of the bar which is ‘EGG SHAPED’ .
- Brass spacer to provide resiliency.
- Provides vertical as well as rotational movements.
ADVANTAGES OF DOLDER BAR
- Bar and rider are available in two heights. Standard size- 4.65mm in height, Micro size-3.6mm in height.
- Rider and bar available in many lengths.
- Bar can be bent and shaped to any configuration.
(Prof. Dolder emphasizes that Dolder bar should be bent to conform to ridge and rider should be segmented to fit straight section
DISADVANTAGE
Bulky-bulky has negative effects on the esthetic result.
Expensive.
(Used for OD- but it is not highly recommended because of the bulk, cost and esthetic problem.)
(Bending etc – require annealing to restore the same strength and restore crystalline structure ).
Procedure of using Dolder bar
Make the abutments with a single path of insertion
Complete the cast of post copings
Try in post copings in the mouth take a full arch pick-up impression
Pour the model
Fab special tray, do border molding, sec impression
Prepare master cast
Prepare occlusal rims
Register the jaw relations, and finish wax set-up and try-in in the mouth
Return wax set-up to the master cast
Make plaster or putty labial, buccal, and occlusal keys or indexes
Remove the keys or indexes and the wax set-up from the master cast
Cut the bar to the desired length.
Invest the abutment retainers and bar in soldering investment
Reseat bar on master cast
Fit the sleeve to length by cutting between the weld points
Fill any space between the bar and ridge with plaster and also bring the plaster halfway up the height of the female sleeve creating space for function of the attachment
Reposition the plaster keys or indexes with teeth on the master model. Prepare the wax set-up of the prosthesis for acrylic processingàInvest, finish
Remove the plaster after polymerization. The segments are now free for activating
Any retention improvement is achieved by embedding a tiny instrument between the acrylic base and the absolute female sleeve.
HADER BAR ATTACHMENT
Consists of prefabricated plastic forms (plastic bars and clips).
Can serve as unit and joint
Plastic Bars-Key hole in shape (greatest bulk being 1.9mm round section).
Bars can be cast in any restorative alloy.
(Non parallel abutmentsàcast with one and solder other.)

ADVANTAGE
Bars can be fabricated in any alloy.
If more retention needed-metal riders can be used.
DISADVANTAGE
Riders are too bulky.
Rider retention decrease rapidly.
No tension adjustment.
(Plastic rider clips serves as good intermediate ‘training clips’ until metal riders can be substituted).
ACKERMANN BAR ATTACHMENT AND CM CLIP ATTACHMENT

Both are same in design.
In this riders are clips that have retention wings-help in easy engagement of rider into the acrylic.
Rider is 2.7mm high and 2.6mm long.
Clip is used on 3 types of bars.
Round bar- 1.8mm, Oval bar- 1.5-2.5mm, Egg shaped bar-1.65 by 2.5mm
Consist of rounded bar will be soldered to the post copings and a clip that fits over the bar. Spacer are provided (.5mm copper sheet) so that clip will not directly contact with the bar and provide some degree of movement.
ADVANTAGE:
- Increased retention in acrylic due to wings.
- Spacer provides resilience and rotation (rotation alone if spacer not used).
DISAVANTAGE:
Bars can be only 1.8mm to 1.9mm in diameter.
Ideal for OD and particularly for resin pick up in the mouth because of retention wings orientation.
OTHER ATTACHMENTS NAMES
BAKER CLIP:
No retention wings (So solder wire for retention.).
14 gauge bar and 12 gauge bar.
Rest is same like CM Clip.
Not recommended since no retention.
MP CHANNELS :
Not recommended.
MAGNET ATTACHMENTS
In order to overcome the problems associated with mechanical attachments, efforts to employ magnetic attachments were made. Magnetic attachments dissipate lateral forces preventing them from being transferred to the abutment.
Previously magnets used for dental purpose were either ALNICO or Cobalt-Platinum magnets. But their permanency was less and there was a lower limit to their physical size (They can not be made too small and still retained a high field strength.).
After 1977 rare earth metal magnets Cobalt – Samarium and Neodymium –iron –boron type were introduced. It became possible to produce magnets with small enough dimensions for dental applications and still provide the necessary forces.( Shriner magnet system by Saco)
Qualities of magnets which are required in dentistry are:
a) Strong magnetic field.
b) Magnetic permanence.
c) Durability and compactness.
2 ways in which magnets can effect tissues:
i ) Physical effect:-because of presence of magnetic field gradient.
ii) Chemical effect:-local or systemic, from the alloy itself, its wear particles or corrosion products, or a systemic effect following their ingestion.
Behrman(1960),Toto and Choukas(1960):- Magnetism is completely innocuous to tissues.
Roth (1968), Becker (1963):- Damaging tissue effects of magnetism were noted but only with magnetic fields considerably stronger than those associated with the dental use of magnets.
Lamb et al., Morin and Daniel:-The dental use of Cobalt-Somarium magnets is most unlikely to cause any harm to tissues.
The first devices used were of an “open field type” (though safe but still if at all possible eliminate magnetic field). In which 2 magnets were used once in the jaw and the other in the denture. In this configuration, the magnets were unshielded and hence magnetic field was experienced in the oral cavity.
Due to concerns about possible effects of magnetic fields on the tissues nowadays “closed field type” systems are used.
In this system, a Ferromagnetic material like stainless steel or Pd-Co-Ni alloy, which is known as Keeper is placed into the tooth rather than a magnet. Paired magnets are placed in the denture. In this configuration (the magnetic field lines are shunted through the keeper as it is in the path of minimum energy and hence) there is no magnetic field experienced in the oral cavity.
Attachments of this type are more efficient as both the north and south poles can be employed for attachment to the keeper, as opposed to the Open field systems, where only one pole is used.
(Paralleling is unnecessary and attachment greatly reduces the load to the roots should the denture move laterally or rotationally).
‘Saco’ magnetic ball slide attachment: Magnetic retention unit-developed at University of Sydney.
Paired magnet and attached keeper and detachable keeper (1.2mm thick)-magnet covered with 0.25 mm thin magnetizable alloy plates to prevent corrosion.
CLINICAL PROCEDURES
Three different procedures can be used to fix the keeper element (detachable keeper) to the root:-
i) Keeper element can be cemented into the oral cavity prepared into the root face.
ii) Can be held with self threading pins.
iii) A root cap and post casting can be made of magnetizable casting alloy.
PROCEDURE FOR CEMENTED KEEPER
Keeper element is an oval disk-5mm long, 3.2mm wide and 1.2mm thick. It has a flat upper side and curved lower side (this face is inserted into the prepared cavity.).
Tooth anaesthetized
crown removed (leaving 1-2mm of crown (tooth structure) above gingiva
Endodontic treatment done
wheel diamond used to flatten the surface of tooth. (gingival trauma can be avoided by removing diamond from edges.)(Root faces need not be coplanar or at right angles to the long axis of the roots.)
Root canal penetrated to depth of approximately 3mm using small round bur-cavity then enlarged in small increments using round burs in ascending sizes.
using straight tissue bur –enlarge cavity in Bucco-lingual direction into oval shape(keeper loosely fit, depth of cavity approximately 1.5mm,walls parallel.).
Using inverted cone bur-undercuts given in buccolingual axio-pulpal line angles.-keeper can not be cemented into the cavity. (parallel cavity walls and undercuts provide ample retention.)
Before cementation-keeper element tested in the cavity for ease of fit to ensure that it can be placed with flat face level with flattened root face
For this, retention element is used as a magnetic handle and is gripped with tweezer. A small square transparent matrix strip is placed between the retention element and keeper to provide separation.
cementation is done using resin cements (Matrix strip provides separation), excess cement removed. then tooth polished with pumice.
Incorporate paired magnet and attached keeper in the denture. Two ways:- Chair side and Lab (transfer coping technique).
Chair side
Keep retention elements in position
take impression
magnets in impression
remove magnets
pour cast
on cast, fabricate conventional denture
curing
chairside – attach magnet, increase the groove with bur
place cold cure
place magnet on tooth
place denture, wait for cold cure to set(make hole in denture for excess to go out).
lab step
take pick up impression of magnet
before cast poured extra transfer keepers given
placed on magnet
cast poured
special tray fabricated
jaw relations taken
dewaxed
during processing magnet stabilized with cyanoacrylate cement
processed
SUB MUCOSAL VITAL ROOT RETENTION
It is an attempt to eliminate some of the basic problems with OD abutments like caries, periodontal and Endodontic problems.
Many patients can not change their oral hygiene habits to properly maintain the gingival sulcus or tooth surface. For these patients a method of root retention and ridge preservation not requiring tooth and oral tissue cleanliness may be the treatment of choice.
GARYER et al. (JPD1980:368-373) did a three year study on 10 patients –they retained 45 roots out of that in 36 roots there was no pathosis).They concluded that sub mucosal vital root retention is one means of eliminating oral hygiene problems while possibly delaying residual ridge resorption.
Existing restoration, gross decay etc removed from teeth to be sectioned. Marginal internal bevel incision is given to remove diseased sulcular epithelium and leaving healthy gingival complex to permit adequate tissue coverage. Following initial incision –deep sub periosteal dissection of adjacent tissues done, thus freeing sufficient tissue for loose wound-edge approximation.
Teeth isolated sectioned 0.5mm above the crestal bone using high speed drill(bur)(large round bur and copious fluid lavage is must)-pulpal tissue observed for bleeding patterns (diseased tissue-profuse bleeding).final tissue coverage and suturing(horizontal mattress suture)
denture relined in areas of surgery and placed; all teeth are sectioned and contoured to existing residual bony ridge form.
Retained root exhibited with complete formation of an osteocementoid plug over the coronal surface of the root and a healthy viable pulp tissue.
ADVANTAGE
1).Reduced cost
2).Prosthesis can be constructed even in bad oral hygiene condition.
3).Preservation of alveolar ridge.
DISADVANTAGE
1). Retention not increased appreciably and also looses the stability provided by vertical walls of the abutment.
2). Development of dehiscence over the roots and pulpal pathosis.
3).Attempts to gain retention from the teeth through some form of attachment are no longer possible.
REMOVABLE PARTIAL OVER DENTURE
Benefit of this OD is that we change a free end saddle or tooth tissue supported RPD into a simple, tooth supported RPD.
Situation in which patient had maxillary right second and third molar and maxillary left premolar and first molar.(maxillary right canine is predominantly compromised).Without this root – Kennedy class IV design – which require support of both tooth and soft tissue – this could result in tipping of the denture around the fulcrum, which would be between the remaining most anterior abutment. Effects of clasp movement in this situation could damage the supporting structures of the remaining clasped teeth. Canine is retained – Endodontic treatment done – short dome shaped coping – the retained root allowed the placement of the anterior fulcrum line in a position that resulted in an tooth supported ROPD. If second molar- periodontally compromised – Hemisection – short coping – class II – classIII.
OVERDENTURE PROBLEMS
1).Abutment loss:
a) Periodontal disease-most common cause-recall every three months.
b) Caries-next common.
c) Failure of Endodontic treatment-Rare.
2).Fracture of denture or perforation of denture: Inadequate reduction of abutment so denture thin in that area.
3). Perforation of coping: At least 1mm thick on occlusal surface.
SUMMARY
Use of overdenture therapy has many advantages like decreased resorption, increased patients manipulative skills in handling the denture and increased retention of denture. Caries susceptibility of abutments, extra cost involvement in the treatment and frequent fracture of dentures are some of the disadvantages of OD.
Proper case selection and abutment selection is an important factor for fabrication of successful OD. Abutment tooth should be situated bilaterally for proper stress distribution.
Construction of a definitive OD requires special attachments or casting. These procedures are time consuming so Immediate OD and transitional OD can be reliable prognostic aid and a prerequisite to the more sophisticated technique.
Abutments can be with coping, without coping or with attachments.
Various stud and bar attachments have been described.
Magnets can be used as attachments in OD. They offer many advantage over the mechanical attachments as they serve to dissipate lateral forces preventing them from being transferred to the abutment.
CONCLUSION
Although improvements in methods and upgraded materials have offered to more approving treatment outcomes, caries and periodontal problems still remain a warning to OD duty life.
In whatever circumstances this type of denture is prescribed unless the patient is prepared to put considerable effort with effective plaque control and maintenances of better oral hygiene, the advantage of this form of treatment will be short lived.
click here to know a new classification of attachments
Pingback: Implant Overdenture - MISCH Complete Notes - extooth
Priya
1 Aug 2020Mam tysm for ur precious ..notes and lecture..most imp is that u r giving free lecture ..u r really great tysm
Fathima Shibli
28 Jan 2021Thankyou ma’am.