IMPLANT OVERDENTURE
Dentures that are stabilized by implants and may be removed by patients are termed as implant-supported overdenture.
The retentive elements are housed in the impression surface of the denture and are attached to the abutment which is secured by implant fixtures. The simplest system consists of either a ball or a retaining cap or a magnet with keeper located upon a single implant. Alternatively, two or more implants may be connected by a bar over which is placed a retaining secure or a dip.
The treatment is frequently used for the retention and stabilization of complete mandibular dentures. In cases where advanced bone loss, from periodontal disease or continuing ridge resorption, results in an unfavorable supporting base for denture the positioning of a limited number of implants can offer considerable stabilization to the denture.
ADVANTAGES
- Traditional over dentures must rely on the condition of remaining natural teeth. The position of these teeth is highly variable and they are often compromised from bone loss associated with periodontal disease. For a mandibular implant-supported overdenture the implants may be placed in planned specific sites. In addition, they are healthy, rigid and provide excellent support.
- Minimal bone resorption occurs with the placement of implants. After the extraction of mandibular teeth, there is an average of 4mm vertical bone loss during the first year following treatment. This bone loss continues over the next 25 years with the mandible experiencing four fold the vertical loss as compared to maxilla. The bone under an overdenture may lose as little as 0.6mm vertical bone over a 5 year period.
- A mandibular denture may move up to 10mm during the function. Under these conditions designed occlusal contacts and the control of masticatory forces are near impossible. An overdenture implant provides stability to the prosthesis and the patient is able to consistently reproduce centric relation occlusion. An overdenture implant-supported overdenture may limit lateral movements & redirect forces more longitudinally thereby minimizing soft tissue abrasions and rapid alveolar ridge resorption.
- The chewing efficiency with an overdenture implant is improved by 20% compared with a conventional complete denture. The maximum occlusal force of a denture patient may improve to about 300% with an implant-supported prosthesis.
- The mandibular implant overdenture often moves with mandibular movements and speech. The contraction of Mentalis, Buccinator, and Mylohyoid muscles may lift the denture off the soft tissues. As a consequence, the denture may lift up producing clicking noises. The retentive implant overdenture remains in place during mandibular movement. The tongue and perioral musculature may assume a more normal position as they are not required in the mandibular denture movement.
- The implant overdenture may reduce the amount of soft tissue extension of prosthesis. This is important for new denture wearer & these who have a low gag threshold.
- Fewer implants are required, as soft tissue area may provide additional support.
- Fewer prosthetic appointments & shorter durations are necessary for removable restorations. Abutment does not require specific location of placement since prosthesis can completely cover the implant abutment.
- Hygienic condition & home maintenance are improved compared to conventional removable prosthesis. Compromise in speech is not present as denture may extend to soft tissue in maxilla.
- An implant overdenture may be removed at bedtime to reduce the effect of natural Para-function which increases stress on the implant support system. It may provide stress relief between the superstructure and prosthesis, and the soft tissue may share a portion of the occlusal load. The prosthesis is usually easier to repair than fixed restoration.
- Shorter restorative appointments, reduced laboratory fees and fever implants allow restoration of patient at reduced wax compared to fixed prosthesis.
DISADVANTAGES
The primary disadvantage of an overdenture is related to the patient’s desire. Some patient’s desire fixed prosthesis as they exhibit psychological apprehensiveness towards removable prosthesis. An implant overdenture would not satisfy the psychological need of these patients to feel the prosthesis is a part of their body.
- Lack of inter arch space makes an implant overdenture system more difficult to fabricate than porcelain to a metal fixed prosthesis. Either an osteoplasty to increase interarch space or a fixed restoration is indicated.
- More time-consuming procedures if attachments are also used along with implants.
- Increased cost compared with a conventional overdenture prosthesis.
CLASSIFICATION OF IMPLANT SUPPORTED PROSTHESIS
FIXED PROSTHESIS
FP-1 PROSTHESIS:
Here the fixed prosthesis replaces only the crown and looks like the natural teeth of the patient.
- It is most often desired in the maxillary anterior region with the implant abutment being 4mm in diameter and round in cross-section.
- The restorative material of choice for an FP-1 prosthesis is porcelain to noble-metal alloy.
FP-2 PROSTHESIS:
Here the fixed prosthesis replaces the crown and a portion of the root. Crown contour appears normal in the occlusal half but is elongated\hyper contoured in the gingival half. This is because the volume and topography of the available bone dictate a different vertical implant placement, i.e. more apical to the cementoenamel junction of the natural teeth.
FP-3 PROSTHESIS:
Here the fixed prosthesis replaces the missing crowns and gingival color and portion of the edentulous site. This prosthesis often uses acrylic denture teeth and gingiva, but maybe porcelain to metal.
REMOVABLE PROSTHESIS:
RP-1 PROSTHESIS:
This type is completely implant-supported or tooth-supported. The restoration is rigid on insertion and overdenture attachment usually connects the removable prosthesis to a low profile tissue bar or superstructure that splints the implant abutments. It may have the same appearance as FP-1, FP-2 or FP-3 prosthesis.
RP-2 PROSTHESIS:
It is a removable prosthesis combining implant and soft tissue support, with the amount of implant support being variable. The completely edentulous mandible overdenture may have two anterior implants independent of \ splinted in the canine region to enhance retention.
OR
Three splinted implants in the premolar and central areas to provide lateral stability.
OR
Four implants splinted with a cantilever bar to reduce abrasions and to limit the amount of soft tissue coverage needed for support.
CLASSIFICATION OF OVERDENTURE MOVEMENTS
Many types of precision attachment may be used in implant overdenture and accordingly, the following range of motions of attachments has been described.
- Occlusal
- Gingival
- Facial
- Lingual
- Mesial Or distal.
- Distal.
However, the actual over denture movement may be completely different when independent of an attachment. In addition, prosthesis movement may vary from above 1 to 6 directions even though the same type of attachment is used.
CARL E. MISCH has sorted implant overdenture movement in six directions or range of movements rather than attachment directions, and the prosthesis movement is evaluated when the restoration is in the mouth.
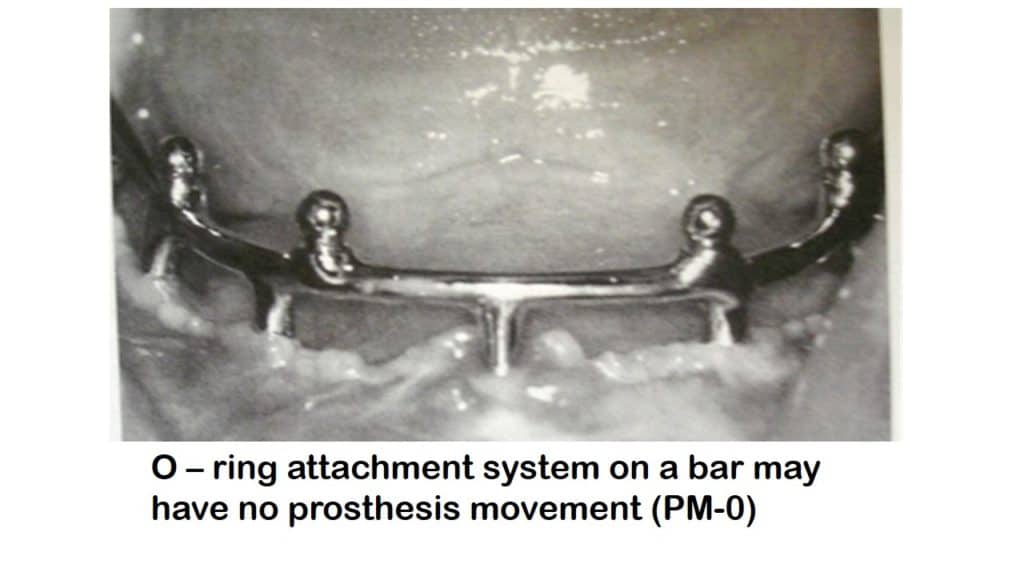
a) PM-1 prosthesis – If prosthesis is rigid whole in place but can be removed when desired.
Eg- O-rings when placed on a complete arch bar in four different sites and prosthesis rest on superstructure bar.
b) PM-2 Prosthesis – A hinge-like a prosthesis movement permitting action in two planes.
Eg – The Header bar & clip is a type 2 attachment. When this system is placed perpendicular to the axis of prosthesis rotation, the prosthetic movement will be in two planes.
- PM-3 Prosthesis – Prosthesis with an attachment system that allows vertical movement and a hinge motion.
- Eg – Dolder bar and clip placed perpendicular to direction of Prosthesis rotation.
- PM-4 Prosthesis – This is rarely indicated for an overdenture system.
- PM-5 prosthesis – This allows a range of motion in an occlusal, mesial, distal, facial and lingual direction. Eg – A magnetic attachment system. However, the implants usually must be independent for this range of motion. If superstructure connects implants, the range of motion decreases.
- PM-6 prosthesis – This allows movements in all six directions. Eg – “O”-ring or ERA attachment.
ATTACHMENTS FOR IMPLANT OVERDENTURE
REQUIREMENTS:
- The female portion of the attachment (matrix) in the prosthesis should be designed to wear and be replaced but not the male portion (patrix) which is connected to the superstructure.
- The attachment should offer the possibility to control the degree of rotation.
TYPES OF ATTACHMENTS:
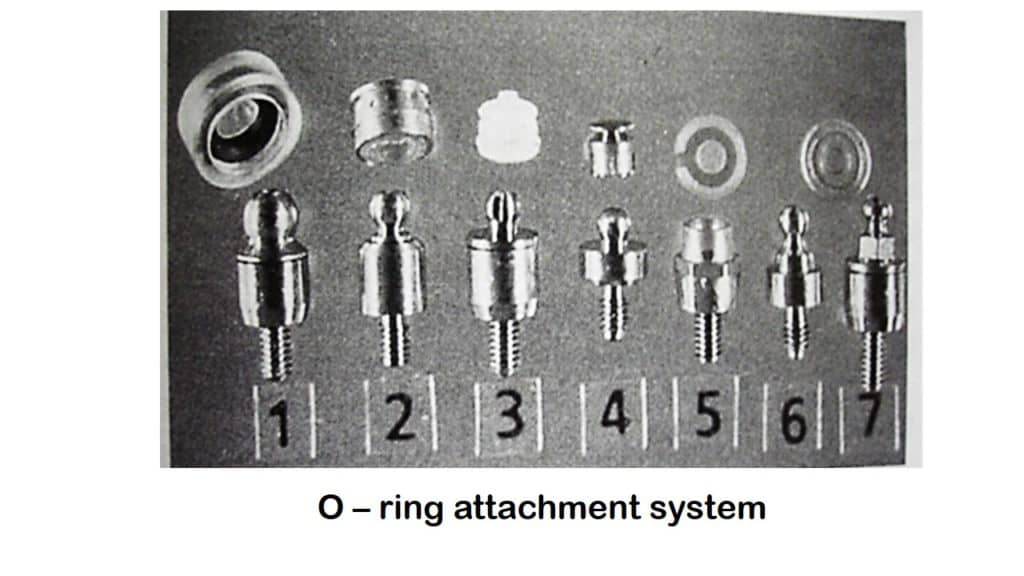
O-RING ATTACHMENT:
It was originally made with natural rubber. The latex was heat treated with sulfur (vulcanized) to improve its properties. The resultant polymer called “POLYISOPRENE” is still used for industrial purposes.
ADVANTAGES:
- Ease in replacing the attachment.
- Offers a wide range of movement with different degrees of retention.
- Affords possible elimination of time and cost of a superstructure for the prosthesis.
DESIGN:
O-RING is a doughnut-shaped synthetic polymer attachment that possesses the ability to bend on the application of load and returns back to its original position when the stresses are relieved.
It is attached to a post with a groove or undercut area so that it does not flex. It has seen a resurgence in popularity with the introduction of ENDOSTEAL type of implants and is widely available in a variety of implant systems.
PROSTHESIS MOVEMENT WITH O-RING ATTACHMENT:
An O-ring is compressed radially between two mating surfaces comprising a post and a metal encapsulator. Based on the movement it permits it is classified as
O-RING
STATIC DYNAMIC
(permits little or no movement (permits reciprocation, rotation
eg: Gasket, Washer) oscillating motion )
METAL ENCAPSULATOR:
- Permits easy replacement of the O-ring after wearing or damage, thereby eliminating chair side realignment.
- It is important that O-ring volume be larger than the internal cavity (an undercut region housing the O-ring attachment).
- The overall size of the encapsulator is larger than O-ring and should be placed on the O-ring post during the fabrication of the prosthesis.
- In general soft metals like aluminum, Brass, Bronze, and Gold should be avoided for metal encapsulator. Stainless steel is recommended as it is softer than the O-ring post to avoid scratching /wearing of the ball.
O-RING POST:
It is usually made of machined titanium alloy or cast precious metal in the root form of overdenture prosthesis.
The post has three parts namely:
HEAD: it is wider than the neck and the O-ring is compressed over the head during insertion.
BODY: is connected to the implant abutment or superstructure
NECK: is an undercut region where the ring seats after it stretch over the head.
O-RING
SIZE:
a) O-ring
and posts may come in variety of diameters depending upon the space available.
- The inside surface of the O-ring rides against the post neck or groove.
- The O-ring internal diameter is smaller than the post neck and fits snugly in the groove diameter.
- The O-ring diameter will be stretched to 1-2 % (not exceeding 5%) when in place against the post neck.
- Was developed by HEMET HAYDER in 1960`s.
- DONEL, STAUBLI modified this system to form the HADER (EDS) system which is only 3 mm in height as compared to 8.3 mm of conventional bar.
- The clips have three different retention strengths and a 20-degree clip rotation which greatly improves the flexibility of the system.
- Gold plated stainless steel housing maintains the clip and reduces the need to attach new system via auto polymerizing resin.
- The standard EDS bar has and superior aspect and an apron below. The apron acts as a stiffener to improve the strength of the bar and li it’s flexibility.
OVERDENTURE TREATMENT OPTIONS:
Implant overdenture range from implant prosthesis deriving support primarily from the soft tissues to a completely implant-supported prosthesis with rigid retention.
The overdenture treatment is frequently used for stabilization of complete mandibular denture in cases where there is extensive resorption of the residual ridge which results in unfavorable support to the denture. Positing of a limited number of implants can offer considerable stabilization of the prosthesis.
A common design in mandibular arch is to position 2 fixtures in canine and premolar area securing 4mm to 5.5 mm abutments to carry 4mm gold alloy cylinder. Soldered between cylinders is a straight platinized round or oval gold alloy bar to which a clip or sleeve is attached. This bar permits some vertical translation and rotation of denture.
Linking the cylinders with a curved bar is unlikely to provide rotation and increase the leverage on the implants. Improvement in the mechanical stability may be provided by extending two cantilever arms distally in line of vertical rotation. Cantilevers of less than 8mm are considered ideal.
MANDIBULAR IMPLANT OVERDENTURE:-
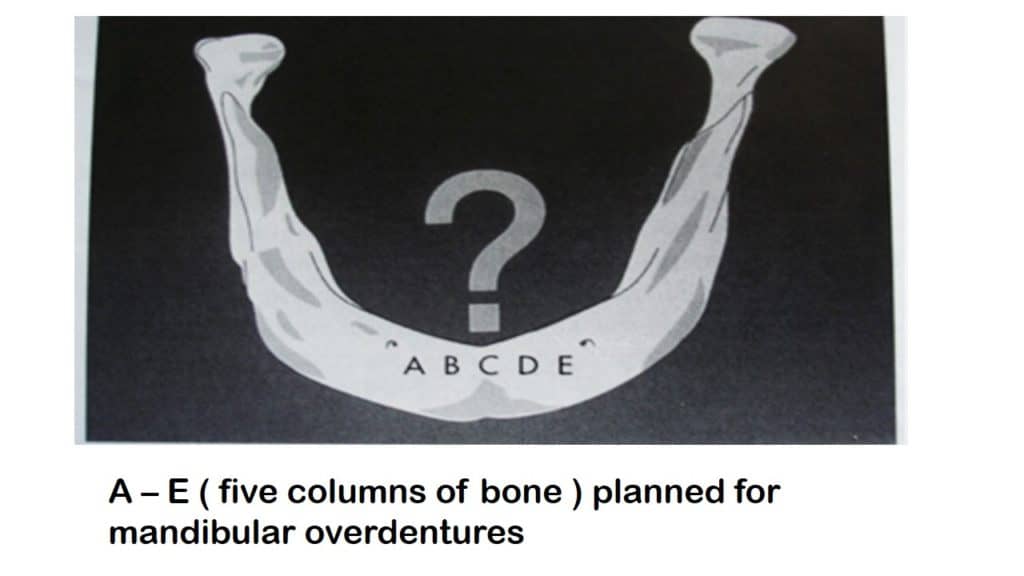
The greatest height of available bone is located in the anterior mandible, between mental foramina of anterior loops of mandibular canal when present. This region usually presents optimal density of bone for implant support. The available bone of anterior mandible is divided into five equal columns of bone serving as potential implant sites. These sites are labeled A, B, C, D & E. All implants site are designed at the time of surgery regardless of treatment option being executed.
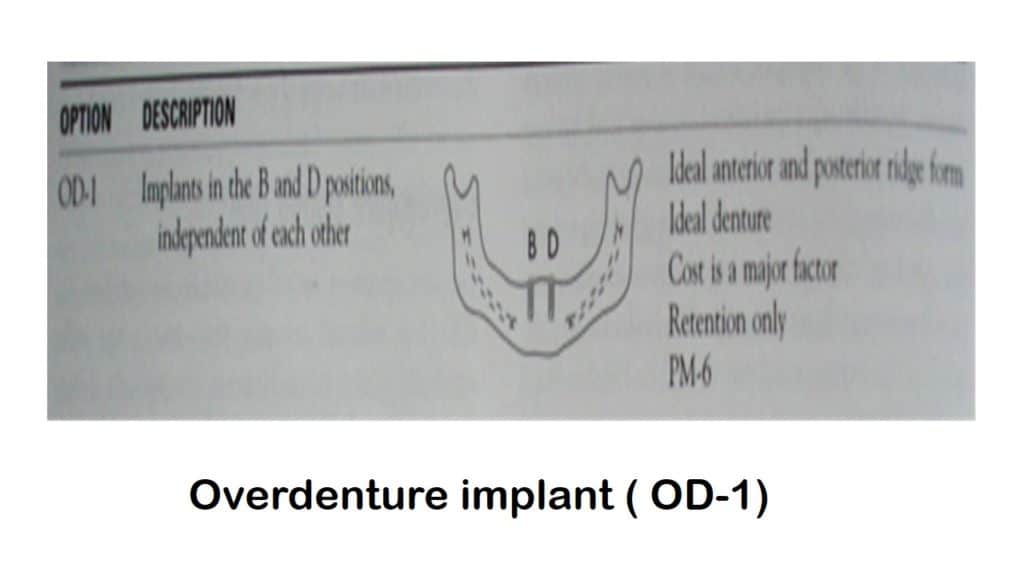
Retention and stability of conventional complete denture may range from good to excellent depending upon the condition of the mandibular ridge. If the posterior arch form is an inverted U shape & lateral stability is good to excellent, the implants remain independent to each other and are not connected with super structure.
OVERDENTURE IMPLANT TREATMENT: OPTION ONE:
INDICATIONS:
- When cost is the most significant factor for the patient.
- The posterior ridge form is “U” shaped with high parallel walls and excellent anatomical conditions for denture retention and stability.
- When the span between the implants is too long and when insufficient space exists to accommodate the attachments or bar.
- In arches that are markedly tapered anteriorly.
- When hygiene maintenance is critical.
Here two implants are placed at B and D positions independently without connecting superstructure. The most common attachment used is O-ring design and the prosthetic movement is PM-6.
Selecting B and D sites for implant placement is critical as it not only reduces the leverage forces acting on the restoration, but also the prosthesis can act as splint for two implants thereby decreasing some stress on each implant.
ADVANTAGES:-
- The primary advantage is low cost.
- The existing restoration may often be adapted with a rebase procedure ground the implants and attachments abutments sites.
DISADVANTAGES:-
- It is relative to poor implant support provided as compared to other options because of independent nature of implants.
- The stability of the prosthesis is primarily gained from the anatomy of the mandible and design of the prosthesis which is like a conventional complete denture.
- Most situations do not allow the prosthesis to act as a splint in true sense, as stress relief attachment provides movement in any direction.
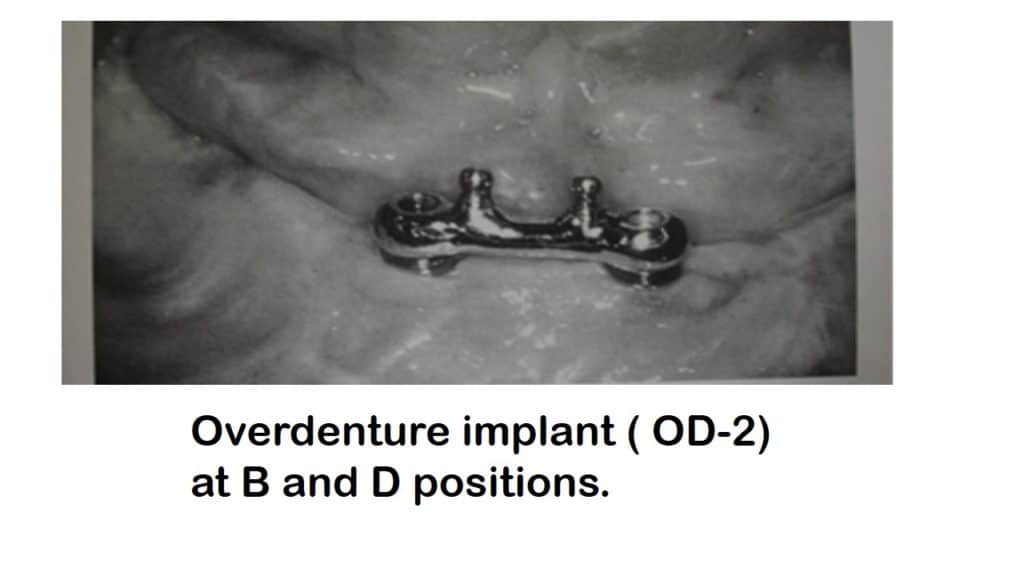
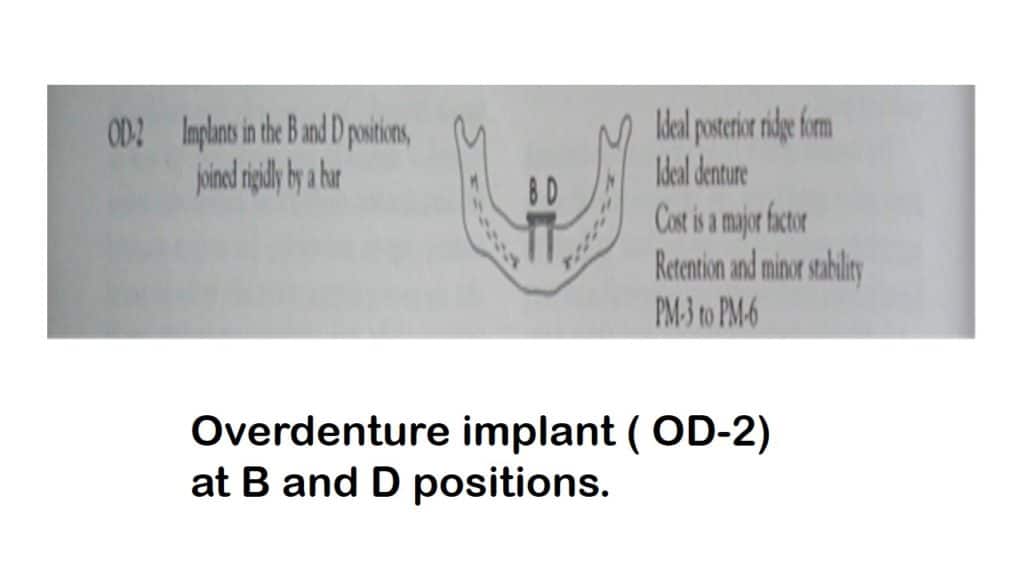
OVERDENTURE IMPLANT OPTION TWO (OD -2):
INDICATIONS:
- The second treatment option (OD-2) is selected only on occasion.
- The patient’s anatomic condition for a traditional denture is good to excellent.
- The posterior ridge is an inverted ‘U’ shape and lateral stability is good to excellent.
- Patient`s complaints are minimal and relate primarily to retention.
- The patient requires new prosthesis and is willing to invest more time and money.
DESIGN:
- The implants are placed in B & D locations & splinted together by superstructure without distal cantilever.
- The retentive element may be an O-ring or clip design depending upon the interarch distance available.
- The bar cross-section is ideally ovoid (DOLDER) or with an apron or any other shape other than round in order to increase its strength and reduce its flexibility. It should be 2 mm away vertically from the soft tissue to provide easy access for hygiene aids. It is usually connected to the facial aspect so that the lingual flange of prosthesis remains within the contour of a traditional denture.
- In addition the bar should be parallel to the plane of occlusion and aligned perpendicular to a line bisecting the angle between the posterior edentulous ridges to allow for rotation of prosthesis (PM-3).
- The 2 splinted implants should not be in A and E positions because of the following disadvantages:
DISADVANTAGES:
- Implants joined with straight bar are lingual to the ridge which causes
i) Difficulty with speech
ii) Anterior tipping of the overdenture
iii) Five times more bar flexure than Band D positions
- implants have to be joined with anterior curved bar
- Greater bar flexibility (9 times than that of Band D positions).
- Increased screw loosening
- Increased moment forces on the anterior aspect of the prosthesis.
- Attachment of a curved bar may prevent prosthesis movement.
- Higher bite force than Band D positions.
- Higher moments of forces may result in bone loss, mobility of the implant or possible fracture of the implant component.
- More lateral load from the prosthesis to the implants than B and D positions.
CONTRAINDICATIONS:
- Highly resorbed C-h type of bone on the posterior aspect of the edentulous ridges.
- Limited interocclusal distance.
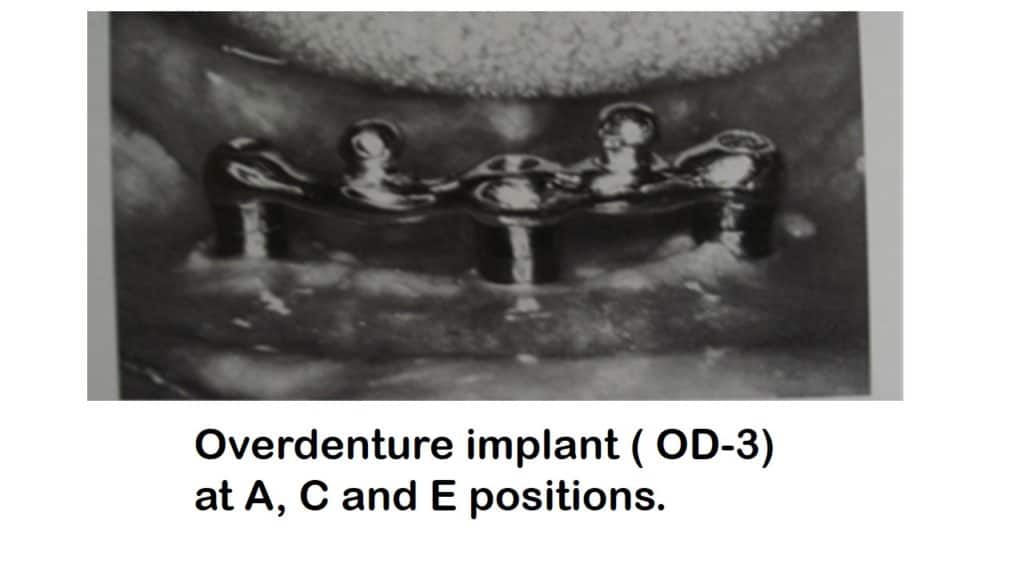
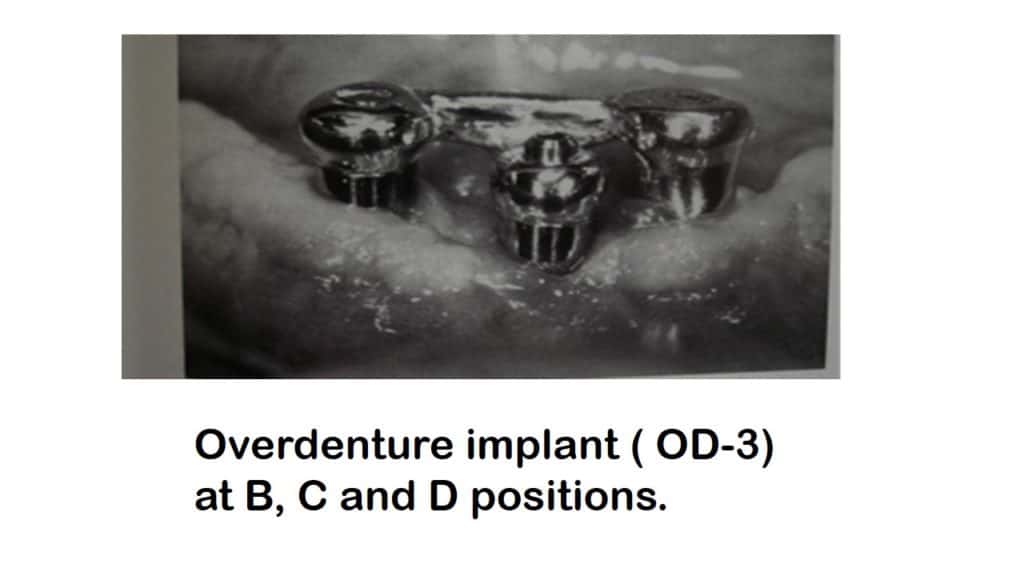
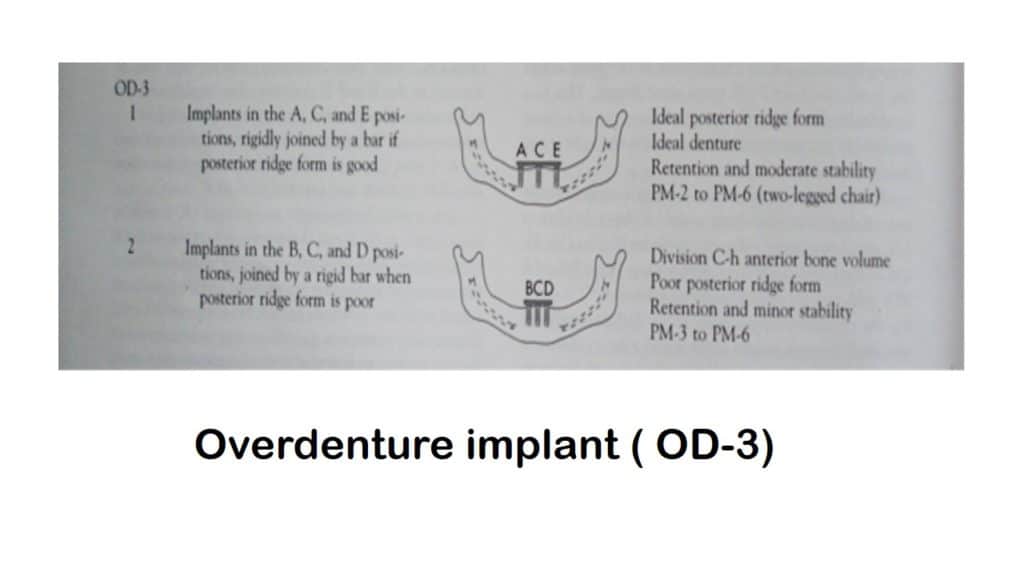
OVERDENTURE IMPLANT OPTION THREE (OD-3).
- In the third option, three root-form implants are placed in A, C and E positions or B, C and D positions (if the anterior and posterior ridge form is poor).
- A superstructure connects the 3 implants but without a distal cantilever. The posterior ridge determines the posterior lingual flange extension of the denture, which limits the lateral movement of the restoration.
- Poor lateral stability places additional force on the anterior implants. The prosthesis movement may be slightly favorable in A, C and E positions and a PM-2 to 6 range of motion is reasonable.
ADVANTAGES:
a) Additional implants provide a six-fold reduction in the superstructure flexure. In addition, screw loosening is less frequent.
b) Implant reaction forces are reduced with a third implant as compared to two implants. The greater surface area allows greater distribution of forces. Three potential implant sites distribute the forces more efficiently and minimize the crestal bone loss.
- There is twice the reduction in moment of force with the three implants in the system than with two implants in A & E regions.
- The restoration benefits the vertical implant support in the anterior arch, and rotation of prosthesis is limited, compared with OD-1 & OD-2. The greater the anterior-posterior distance of A, C and E implants greater is the lateral stability of the denture.
- The prosthesis should not attach or contact the angles formed by a superstructure. This would result in a too rigid system. If an attachment is designed for prosthesis, the bar may connect the facial aspect of A and E implant coping on the lingual side, so that a straight bar perpendicular to path of rotation may be fabricated. A PM-2 or greater prosthesis movement is desired by three anterior implants.
IMPLANTS AT “B”, “C” AND “D” POSITIONS:
a) Implants placed in B, C, D regions are indicated with poor posterior ridge form. The increased horizontal movement of restoration results in greater lateral forces on the implants.
b) There is more freedom of movement for the prosthesis and is greater than PM-3 to reduce stress on implants.
c) placing implants at these three positions increases the posterior movement of the restoration, but decreases the amount of stress on the implant and screw-retained bar.
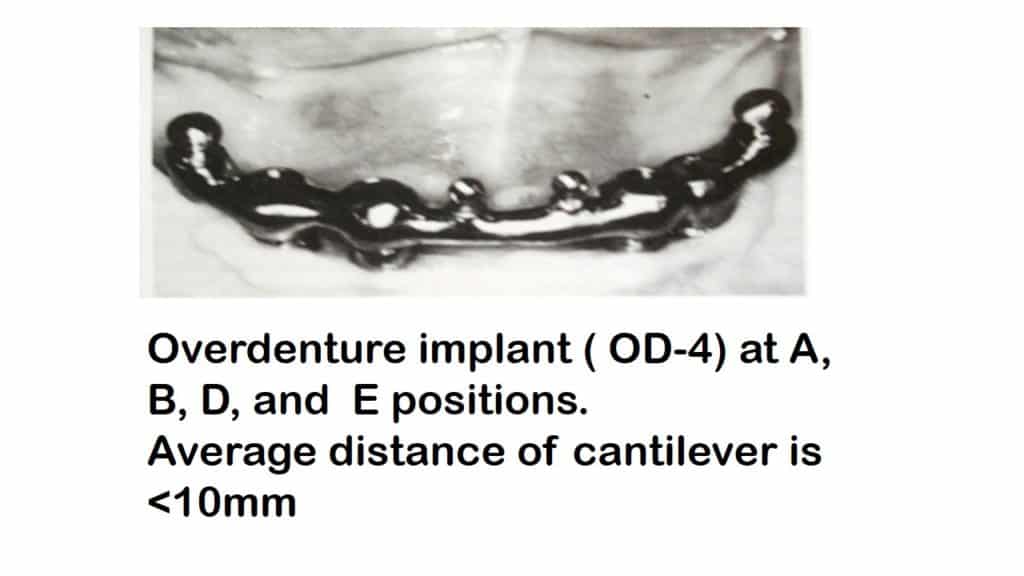
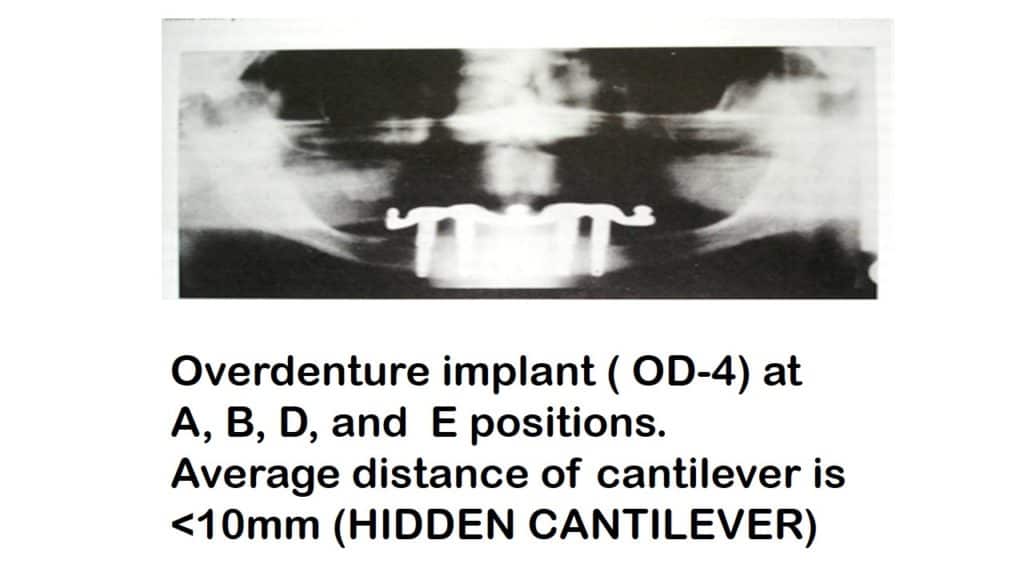
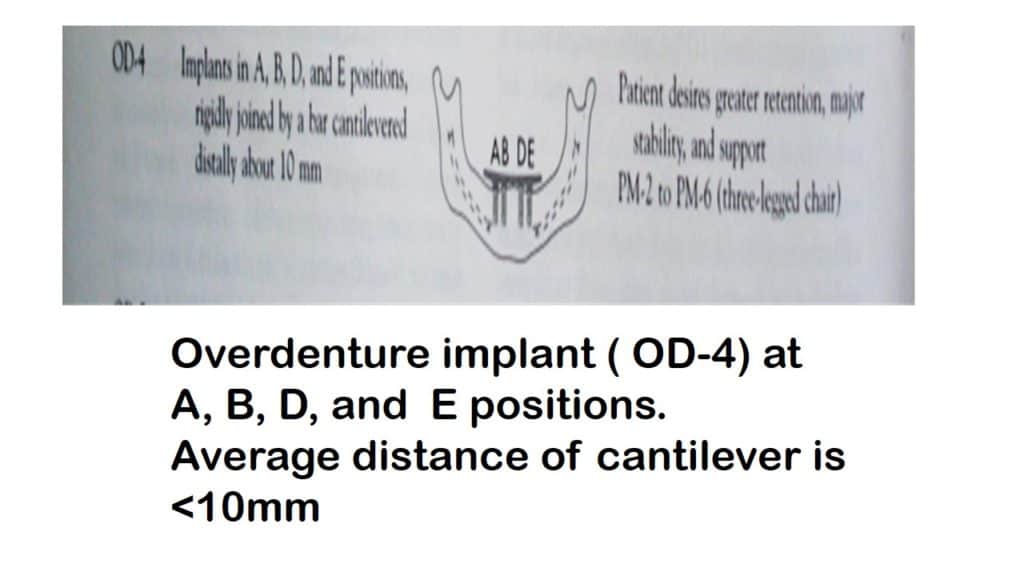
OVERDENTURE IMPLANT FOUR (OD-4)
- Four implants are placed in A, B. D. & E regions.
- These implants provide enough support to distally cantilevered superstructure which extends up to 1.5 times the anterior-posterior distance of approximately 10 mm on each side if the stress factor is low.
- The prosthesis may have more stability and a PM-2 range of motion is most common. The prosthesis is of RP-5 type but has the least support from the soft tissues.
- If clips are employed it must be placed perpendicular to the path of rotation not along the cantilevered bar where it only functions then is retention.
- The actual cantilevered length is determined from the point of prosthesis movement, not the length of the superstructure bar, sometimes the bar may be cantilevered 10 mm beyond the distal implant (HIDDEN CANTILEVER).
INDICATIONS:
- Poor posterior anatomy of the residual ridge.
- Lack of retention and stability.
- Soft tissue abrasions and difficulty with speech.
- Patient`s complaints are more demanding than previous treatments.
- The external oblique line is high and mylohyoid ridge corresponds to the crest of the residual ridge.
ADVANTAGES:
- There are greater vertical support and lateral stability to the prosthesis.
- Cantilever bar provides additional retention of the superstructure, which limits the risk of screw loosening and other complications.
OVERDENTURE IMPLANT OPTION FIVE (OD-5).
INDICATIONS:
a) Designed for patients with moderate to severe problems related to
traditional restorations.
b) The needs and desires of patients are often demanding.
c) In patients whose major concerns are lack of stability, sore spots and inability to wear the denture.
DESIGN:
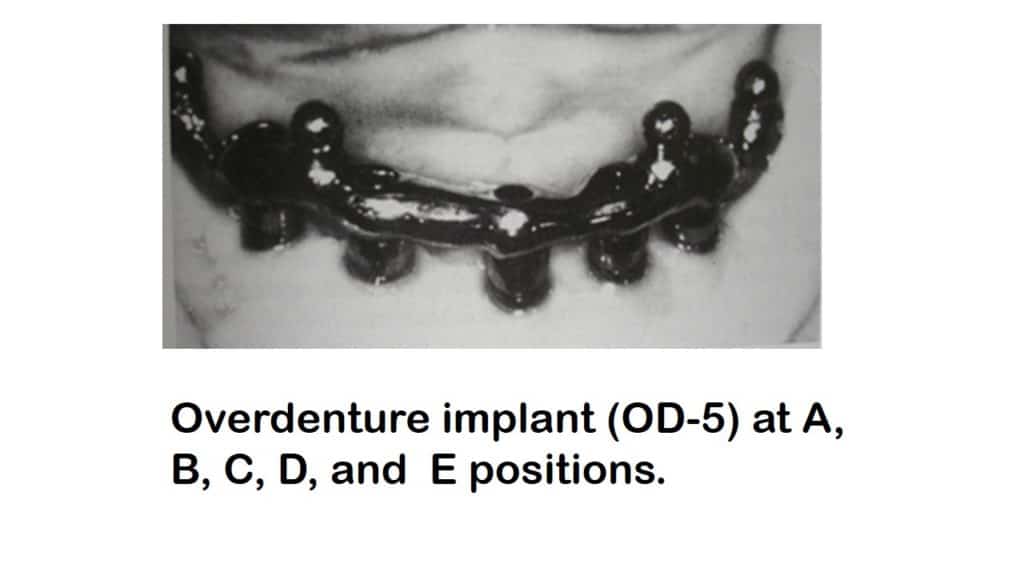
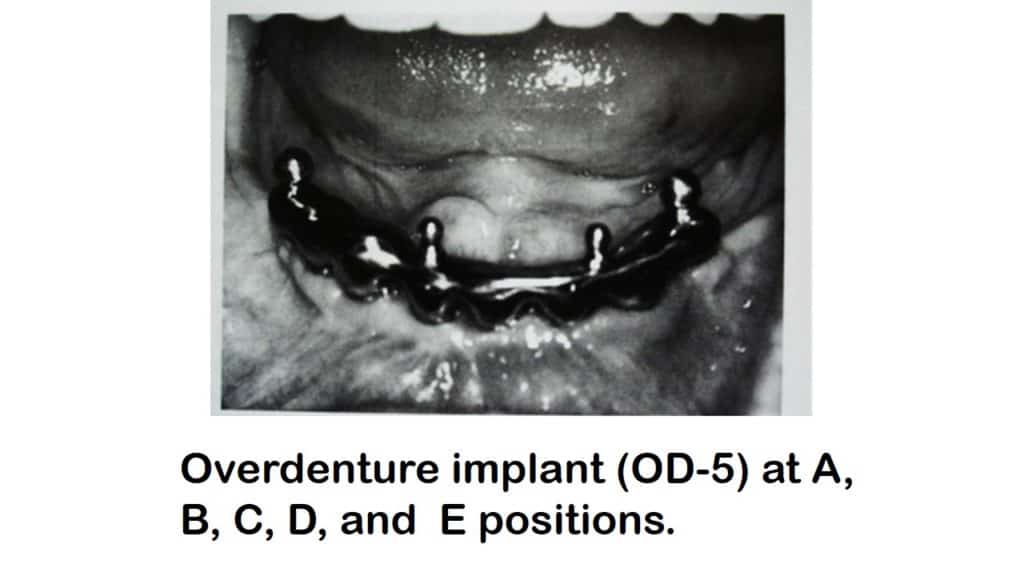
a) The five implants are placed in A, B. C. D. & E. position with a distal cantilevered bar superstructure.
b) The distal cantilever is approximately 15 mm, which places it under the first molar region the restoration does not extend usually beyond the first molar either teeth or soft tissue coverage.
c) The restoration is RP-4, completely implant-supported.
d) The retentive elements \ attachments are typically 4 O-rings which are evenly distributed (two anterior and two posteriors to the distal implants), with a HADER bar clip placed distal to the last O-rings on each cantilevered section.
PURPOSE OF HADER BAR:
- It acts as a back-up system for additional retention in case an O-ring stud breakes, or in case the vertical dimension of occlusion does not permit the use of high profile retentive O-ring.
- It also permits to decrease stress to the bar and implants, if screw loosening or bone loss around the implants is noticed.
- By sectioning the bar, when not required it converts the RP-4 prosthesis to RP-5 prosthesis.
The presence of five implants also allows the superstructure and the prosthesis to be cantilevered forward from the anterior ridge. This is of particular benefit for ANGLE`S skeletal class-II patients. After the surgery is done & implants are placed preliminary impressions are made following a gap of 2-3 weeks to allow healing of tissues.
Approximately 2 weeks after the insertion of implants the mucoperiosteum is sufficiently healed to allow the existing complete denture to be re-inserted, restoring appearance and function. After 4-6 months the final impression may be made. For a final impression, elastomers are advocated.
MAXILLARY IMPLANT OVERDENTURE :
TREATMENT OPTIONS WITH SUB-ANTRAL APPROACH:
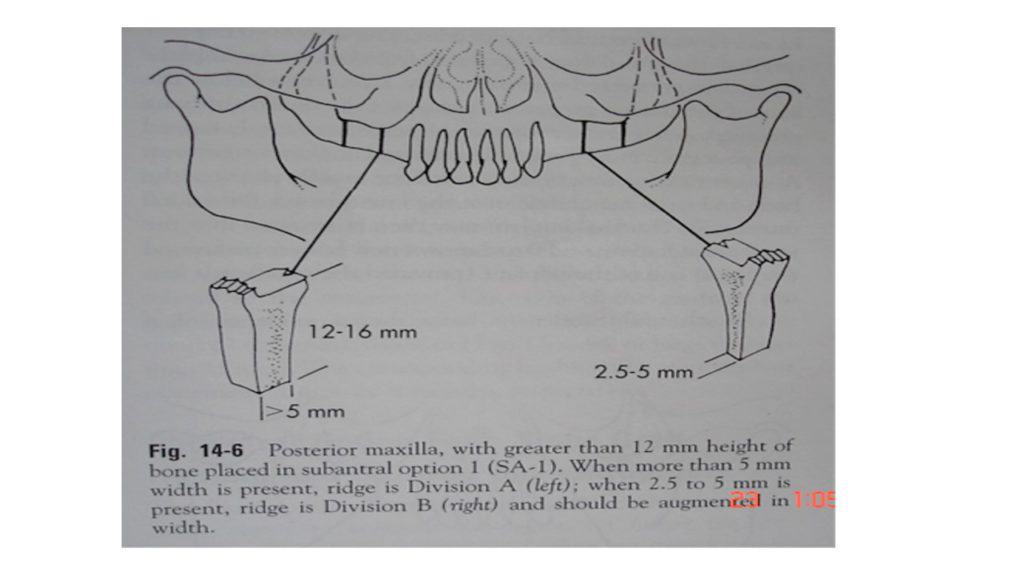
METHOD-I: CONVENTIONAL IMPLANT PLACEMENT:
- This occurs when there is sufficient available bone height to permit the placement of endosteal implants following the usual treatment protocol.
- D2 bone should have at least 11 mm, D3 bone 12 mm and D4 bone 13 mm of vertical height for a 4 mm diameter screw-type implant with hydroxy-appetite coating.
- Narrower bone volume patients may be treated with osteoplasty or augmentation to increase the width.
- Endosteal implants in this category are left to heal in non-functional environment for approximately 4-8 months before the abutment posts are added for prosthetic reconstruction.
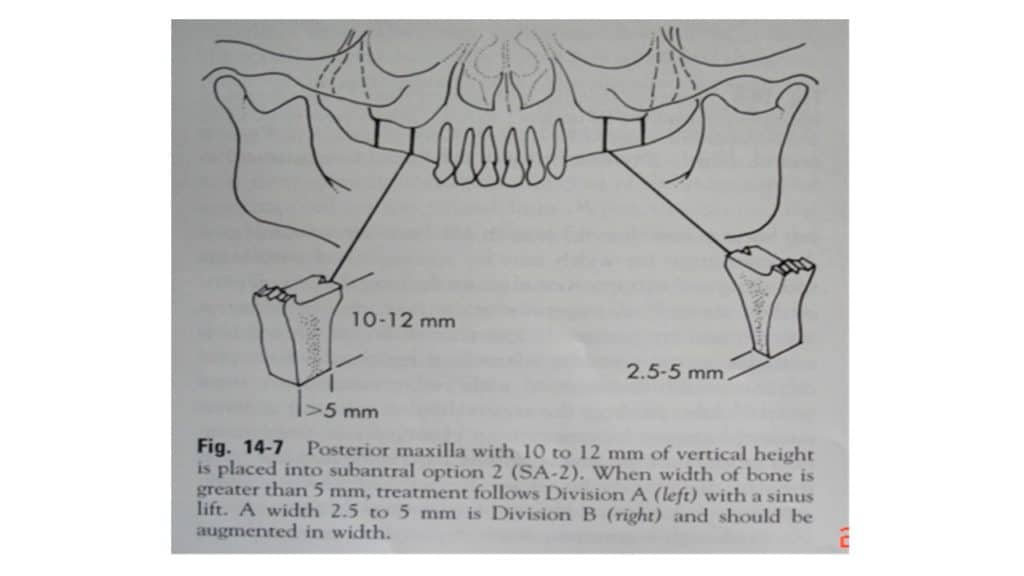
METHOD 2: SINUS LIFT PROCEDURE:
- It is selected when 10-12 mm of bone is presently using screw-type root form implants. To obtain 12-14 mm of vertical bone necessary for implant survival. The antral floor is elevated from below.
- An implant osteotomy is performed approximately 1-2 mm below the floor of the sinus. A flat osteotome is inserted and firmly tapped into position 2mm beyond the prepared implant osteotomy. A greenstick fracture of the sinus floor usually elevates the bone and sinus membrane over the broad-based, flat ended-osteotome.
- The final implant may then be inserted into the implant osteotomy and 0-2 mm of new bone form around the apical end of the implant (provided that the membrane was not torn).
- As success cannot be confirmed at the time of the placement, radiography is used to indicate success (0.2 mm vertical height after 6-8 months after surgery).
OPTION 3: SINUS GRAFT AND INITIAL DELAYED ENDOSTEAL IMPLANT PLACEMENT:
a)It is indicated when at least 5 mm of bone (vertical ) and sufficient width are present between the antral floor and the crest of the residual ridge in the area of needed prosthodontic abutments. A Tatum lateral maxillary wall approach is performed just superior to the residual alveolar bone. After the lateral access window and the membrane are rotated in and upward to a superior position, a mixture of autogenous bone (harvested from the tuberosity area), alloplastic and allograft material is placed in the space previously occupied by the sinus. After 2-4 months, when the area has healed uneventfully, the implants can be inserted. The implant design and surgical approach is similar to other options and the bone density formation is in part related to the transverse width of the sinus in the grafted area.
OPTION 4: SUBANTRAL SINUS GRAFT HEALING AND DELAYED IMPLANT SURGERY:
Indicated when less than 5 mm of bone is present in between the residual crest of the bone and the floor of the maxillary sinus. The compromised osseous bed, extensive pneumatization and insufficient bone structure for primary implant stabilization require more time for bone to replace the graft. The Tatum lateral wall approach is used to gain access to the maxillary sinus, elevation of sinus membrane is done and a mixture of autogenous bone, alloplastic and allograft, with additional graft site being the ramus\symphisis region of the mandible. The augmented region is allowed to heal for 6-8 months before re-entry for endosteal implants and 4-10 months elapse before prosthodontic reconstruction depending on the bone density at the time of implant placement.
POST INSERTION MAINTENANCE OF IMPLANTS IN IMPLANT SUPPORTED OVERDENTURES:
Reports on post insertion prosthodontic maintenance and complications of mandible mucosa and overdenture implant have been documented in several studies.
These prosthodontic maintenance requirements must relate to the design of the overdenture implant and the respective PATRIX and the MATRIX components of the implant system used. With a few exceptions, the majority of maintenance requirements are from the studies on two anterior implants supporting an overdenture.
PATRIX MAINTENANCE:
Wear or fracture of the ball abutment head shape seems less frequent than for gold alloy bars. However, maintenance of the ball abutment-retaining screws, and especially magnetic keepers either in terms of loosening or fractures is high. Progressive manufacturer developments in terms of the ball abutment screw design for the Branemark system and Astra-Tech Dental implant system will no doubt limit this, although it is interesting to note that modifications have not been necessary with the ITI retentive anchors, perhaps because of an alternative design.
MATRIX MAINTENANCE:
The burden of matrix maintenance is paramount to the prosthodontist regardless of whether O-rings, titanium springs, gold alloy caps, magnetic wear, corrosion or replacement, or bar retention clips are considered.
Exchange of rubber O-rings was recommended either annually or biannually depending upon the number of implants used. It appears to difficult to predict the frequency of replacement of rubber O-ring matrices as this depends on whether it was determined subjectively (by the patient) or objectively (by the prosthodontist). No controlled comparative studies between these were found. Determining specific differences between the maintenance of ball, magnetic and bar overdentures has been limited by the extent of the categorizations used. Direct comparison of unique maintenance differences between the titanium and gold alloy matrices is lacking for both the Branemark and the ITI systems, although there is unanimous agreement on the burden of using magnetic matrices.
Reports are dominated by the high burden of clip maintenance in splinted designs. Original and subsequent reports indicate a minimal need for clip activation. Clip activation is also dependent on the patient’s requests for activation together with the objective evaluation by the operator. Loss of retention has been attributed to the demanding nature of the patients who actively sought optimal stability for their dentures. During a multicenter over denture study, it was found that clip adjustments occurred in 47 of the 76 cases (62%) on 111 occasions. Clip fracture occurred in 25 of the 76 cases on 39 occasions. It could, therefore, be interpreted that, even by observing the principles of the axis of rotation, clip fractures do occur.
IMPACT OF THE INTERABUTMENT DISTANCE:
Standardization of the interabutment distance to aid controlled reporting of prosthodontic requirements would be helpful, but the distance seems to have been determined to be in the range of 12-35 mm without any particular standardization. Aspects of patrix and matrix maintenance in relation to the interabutment distance in splinted designs have been discussed by MERICSKE-STERN, who recommends not less than 8-10 mm between abutments to facilitate proper placement of the clips. The shorter the bar segment, the more the chance of the clip loosening in the acrylic resin. A further recommendation, that the length of the bar segments should not be less than 15 mm, is difficult to apply when four implants are used, but satisfactory with three bar segments and matrix length limited by minimal interabutment distance were reported.
RELINES:
The frequency of relines required during follow-up of mandibular mucosa and implant overdentures would appear to vary from 8% -30% regardless of the design. First, no criteria have been used by the researchers on mandible overdentures to evaluate the need for relines as to whether it was based on purely the subjective needs of the patient or on the interaction of both the subjective and the objective needs.
Secondly, few studies have reported any differences in the frequency of relines between splinted and unsplinted designs or between 2,3, or 4 splinted implants. Furthermore, remaking of the mandibular overdentures could be subject to the same criticism, particularly when specific criteria have been used to evaluate replacement of complete dentures.
FRACTURES:
Because of the concern about mandibular implant overdenture fractures during longitudinal evaluation, some authors have used a cobalt-chromium alloy framework. Overdenture fracture has been said not to be surprising because of the large space occupied by the abutments and some retentive elements of the denture. More recently the use of metal framework has been questioned in view of their increased loading on two implants.
PROSTHODONTIC MAINTENANCE AND TIME TO RETREATMENT:
Successful implant overdenture treatment outcomes have been proposed in terms of longevity\survival, physiologic impact, psychologic impact, and economic impact. The overdenture design within the mandibular arch shape, the implant system the patrix and the matrix components used and biomechanical issues clearly influence the time to retreatment. This time can vary between different systems. There is a need for more studies between different systems linking prosthodontic maintenance requirements, cost-effectiveness, and time to retreatment.
SUBMUCOSAL VITAL ROOT RETENTION:
In this procedure, the roots of the teeth that are going to serve as abutments are intentionally retained beneath intact overlying mucosa. Many patients during retrograde periodontal changes due to lack of oral hygiene methods cannot\will not change their oral hygiene habits to properly maintain the gingival sulcus or tooth surfaces that no longer possess enough height to allow the dental hygiene aids to remove plaque and other debris.
For these patients, a method of root retention and ridge preservation not requiring tooth or oral tissue cleanliness may be the treatment of choice (GARVER and his associates).
KROL (1976) stated that the maintenance of alveolar bone tissue has depended upon the presence of healthy root and periodontal ligament with the resultant torsional forces delivered to bone either due to functional or Para functional activity.
PATIENT AND TOOTH SELECTION:
Patient to be selected should be in good health free of any systemic diseases\disorders or they should be under control. Those scheduled to receive an upper denture should have isolated retained teeth between the right and left premolars whereas for mandibular denture two or more teeth are essential.
All the teeth should meet the following criteria:
- No more than 1 mm of horizontal mobility.
- No infrabony pockets that cannot be reduced during surgery.
- Healthy mucogingival tissue for watertight closure of the mucosa.
- Remaining supporting tissue atleast one-third of total root length.
- Teeth should be asymptomatic, test vital, or show only calcific metamorphosis.
PRESURGICAL PROSTHETIC REQUIREMENTS:
- Necessary radiographs should be made of all remaining teeth and tissues adjacent to the alveolar ridge (EVERETT and FIXOT 1963), (LANELY and TOLMAN 1968).
- Recording the vertical dimension of occlusion, the patient’s arc of closure and centric relation may be necessary to enhance esthetics.
- Pre-prosthetic treatment may include relining\rebasing of the existing prosthesis after prosthetic occlusion is obtained.
- In cases where the existing prosthesis is totally inadequate, transitional dentures for patient comfort can be made.
SURGICAL PROCEDURE:
- Patients can be managed well using local anesthesia.
- Existing restorations, gross decay or temporary filling materials should be removed from the teeth to be sectioned.
- Marginal internal bevel incisions around the teeth to be sectioned should be used so that diseased sulcular epithelium can be removed, leaving sufficient healthy gingival complex to permit adequate tissue coverage and watertight closure over the surgical site.
- Following this initial incision, deep subperiosteal dissection of adjacent tissues is performed, thus freeing sufficient tissue for loose wound edge approximation.
- The selected teeth after being isolated are surgically sectioned 0.5 mm above the crestal bone using a high speed surgical drill and a large round bur with copious fluid lavage.
- The pulpal tissues are least damaged if a circumferential sectioning technique is used cutting the pulpal isthmus least.
- Packing of the oral pharynx with gauze or tooth tethering is suggested to prevent the sectioned clinical crown from being aspirated.
- After crown sectioning granulomatous tissue is debrided from around the root, and calcular tags overlooked during pre-surgical preparation are removed.
- Smoothening of coronal root surface is accomplished using a surgical bur and root face is made contiguous with the alveolar bone surrounding the retained root, and the pulp tissue is observed for a bleeding pattern.
- Pulp tissue devoid of copious hemorrhage is questioned in prognosis and should be evaluated closely prior to final soft tissue covering and suturing (GARVER and associates 1979).
- Horizontal mattress type suture is used for initial wound edge approximation, which is followed by a continuous running suture to ensure watertight closure of the incision line.
- This portion of the technique is of great importance because of the position of the sectioned roots immediately beneath the wound edges.
POST SURGICAL CARE:
- The surgical area is packed with gauze pads to prevent immediate post-surgical bleeding.
- Antibiotics and analgesics to control infection swelling and pain are prescribed on an individual basis.
- Simple oral hygiene care, ice pack application are also helpful in controlling post-operative problems.
- At this time, the prosthodontist prepares the tissue for denture adaptation, evaluation, and delivery of the prosthesis. Pressure indicator paste is used to check any interferences and overextensions that would cause dislodgement of the denture.
- Intra-oral chair side harmonizing of the denture occlusion is started. However, as mandible movements are erratic and uncoordinated when the patient has been anesthetized and subjected to this type of surgery, only gross discrepancies between the centric relation and maximum intercuspation of denture’s occlusal surfaces are removed.
- After the swelling has subsided and initial healing has taken place, usually within two weeks after surgery, dentures are remounted to remove all the processing errors and to create a balanced occlusion.
- Patients should be observed weekly for a period of 1 month to evaluate tissue response and patient comfort. Treatment relining material is replaced as necessary until healing is complete.
- At this time the dentures are evaluated for exactness of the fit, reliability during function and fulfillment of the esthetic requirement. The new prosthesis should be fabricated if any of these factors are compromised.
OVERDENTURES FOR CONGENITAL / ACQUIRED DEFECTS AND IRRADIATED PATIENTS.
Many patients with congenital and acquired defects neither can be treated successfully by orthodontic therapy or by surgical intervention nor can they be successfully treated with conventional procedures i.e. either. Fixed or removable.
Congenital defects that most frequently are treated with overdenture include the following:
- Cleft palate\lip.
- Oligodontia.
- Microdontia.
- Cleidocranial dysostosis.
- Class III patients – prognathic mandible.
Acquired defects may result from –
a) Accident causing mal-alignment teeth.
b) Disease e.g. abraded or crowded teeth
c) Misuse.
The objective of overdenture treatment in these cases should be the same as with any other prosthesis i.e. to preserve what remains and to improve function and aesthetics. In addition, good support to the lips and other soft tissue can be provided for many patients. It is seldom necessary to alter existing teeth and the procedure is completely reversible.
The procedure essentially remains the same as for the remote overdenture.
The overdenture in such cases will help in the preservation of bone and additional support can be achieved by the use of non-rigid attachment between the denture and all\ some of the remaining natural teeth.
OVERDENTURE FOR THE PATIENTS WITH RADIATION THERAPY.
Patients who have received radiation therapy to the oral cavity frequently present with a particular concern towards a prosthetic replacement of missing teeth. Oral cancer patients who have neglected their dental care may present with generalized caries, failing restorations, missing teeth, occlusal plane disharmony and periodontal and endodontic involvement of dentition. Treatment planning must reflect total patient consideration such as physical and psychological limitations, the continuing necessity for medical care and attitude towards oral health and hygiene.
Xerostomia, radiation caries, mucosal fragility and potential for osteoradionecrosis may all compromise prognosis with complete denture, or longevity with the fixed restoration. Following irradiation of bone, there is a marked reduction, in the healing potential of bone, because of altered blood supply from obliterative endarteritis which may lead to osteoradionecrosis in alveolar bone.
Because of tooth extractions immediately before, during or after the radiation therapy has been linked to osteoradionecrosis teeth not restorable with conventional operative procedures of fixed prosthetics are excellent candidates for root retention and use as overdenture abutments, and even periodontally involved teeth can be retained to serve as overdenture abutments.
Besides avoiding extractions in irradiated patient, to minimize the risk of osteoradionecrosis, retention of teeth has many advantages in these patients. Retention and stability of the tissue bearing area of the denture are enhanced by the presence of root and the supporting bone, which is important in post-surgical sites or where saliva is thick, ropy or absent. Radiations that include the temporomandibular joint and muscles of mastication may induce trismus, making the dental procedures difficult for both the patient & dentist. Thus root retention for overdenture may be more feasible than other restorative treatments in patients with truisms. Unlike fixed restoration overdenture may be removed for hygiene, observation of adjacent tissues and topical fluoride application.
TREATMENT PLANNING.
Overdentures for the irradiated patients can be planned at any stage in radiation sequence. If planned during pre-radiation therapy screening, periodontal and endodontic preparation may be completed during early weeks of radiation therapy. After the active phase of radiation is completed and tissues have recovered to their fullest extent from accompanying mucositis, Prosthodontic treatment can be initiated.
CLINICAL EVALUATION AND PREPARATION :
Complete resolution of radiation mucositis symptoms and acceptable epithelial surface consistency are critical before beginning the prosthodontic rehabilitation. Bony tissues including residual ridge, temporomandibular joints & existing exostoses are examined clinically and radiographically.
Oral hygiene and periodontal status of the potentially useable teeth are evaluated clinically and radiographically and periodontal procedures are instituted if necessary.
Diagnostic cast are articulated to provide preliminary information on occlusal plane, potential denture space, path of insertion and maxillo-mandibualr relationship.
Potential abutment teeth are evaluated for sub gingival caries and periapical pathosis. Teeth with the marked mobility; supraeruption and soft tissue granulation into the periodontal ligament area are treated. If extractions are necessary antibiotic prophylaxis is instituted and healing is monitored closely.
The path of placement is evaluated for any undercuts on diagnostic cast to avoid pre-prosthetic surgery. Endodontic treatment for teeth to serve as abutments can be done without risk of infectious complications or osteoradionecrosis even in radiated field. Vital tooth endodontics may be performed as they would be for patients without radiotherapy. If a tooth presents periapical lesion radiographically or if there is any chance of forcing necrotic material through apical foramen during instrumentation, treatment should be carried out under antibiotic coverage.
ABUTMENT DESIGN:-
Whether the abutment is prepared before the final denture insertion or at appointment during the insertion of immediate overdenture, they should be prepared to a dome shape, extending 2-3mm above the contour of surrounding gingival tissue and should be sealed with amalgam plug 3-8mm into filled canal. Amalgam plugs are superior to other attachments as they eliminate tissue irritation & also provide for ease of access for endodontic re-treatment or addition of attachments & also allow fluoride application.
PROSTHESIS FABRICATION & INSERTION:
Standard principles & techniques for overdenture can be utilized with special attention given to soft tissue management. Excessive use of heat in border molding & the use of possible irritants such as zinc oxide eugenol paste should be avoided. Rubber base impression material may be used.
At insertion, pressure indicating paste is used to relieve denture intaglio as needed.
POST INSERTION CARE:
All post-irradiation patients should be closely monitored for tissue irritation.
Tissue breakdown must be avoided to protect the underlying bone, which remains in danger of osteoradionecrosis. Ongoing observation of denture bearing soft tissue is necessary to distinguish between denture irritations & early neoplastic lesions.
Patients are seen for post-insertion examination at 24 & 48 hrs & at least once a week until soft tissue condition is stable.
The technique should include a planned reline of the prosthesis after 4-8 weeks to ensure uniform light denture contact with hard & soft supporting structures. All patients required treatment are instructed to use 1% sodium fluoride get with a natural PH of caries control. They are taught to clean abutment with a soft toothbrush.
For patients with xerostomia oral lubricants & artificial saliva can be used. Recall visits should include oral cancer screening & evaluation of prosthesis for occlusion. Guidelines for Prosthodontics treatment of a patient who has received radiation to the head & neck area include avoidance of dental extractions, simplicity in treatment, home care & follow up.
CROWN AND SLEEVE COPING PROSTHESIS.
RATIONALE:
- The concept of crown and sleeve coping prosthesis (removable telescopic partial denture) resulted from clinical experiments with the tooth-supported complete denture at “VALLEY FORGE ARMY HOSPITAL” during 1955-1957 (MILLER 1958).
- This prosthesis utilizes the basic concepts of tooth-supported the complete denture and has been modified to embody the biological contours and splinting principles of fixed periodontal prosthesis with the use of telescopic removable drowns (YALISOVE 1966).
- It is used as a therapeutic modality rather than a more replacement of teeth.
MAJOR CHALLENGES:
- To salvage the remaining abutment teeth.
- To maintain the periodontal attachment apparatus and the alveolar bone support with a type of prosthesis designed to function within the parameters of the weakened periodontal situation (EICH 1972).
DIAGNOSIS AND TREATMENT PLANNING FOR CSC PROSTHESIS:
- Proved to be viable alternative when the negative factors outweigh the positive ones in treatment planning for fixed or conventional removable prosthesis.
- Usual diagnostic procedures are employed with clinical examination (periodontal, endodontic, radiographic and diagnostic casts analysis).
- It is important to establish the sequence of therapy:
- Extraction of condemned teeth.
- Removal of extensive carious lesions.
- Determination of vertical dimension of occlusion.
- Periodontal and endodontic therapy.
- Orthodontic therapy
- Preparation of the abutment tooth after selection.
- Provisional stabilization
DESCRIPTION OF CSC PROSTHESIS.
The prosthesis consists of three components.
The sleeve copings
The secondary crown.
A frame work.
THE SLEEVE COPING:
The sleeve coping is a type III gold alloy casting that protects the abutment tooth and serves as bearing for the secondary crown. The design of the sleeve coping is determined by the periodontal condition of the corresponding abutment tooth i.e., if the tooth is weaker, more tapered abutment preparation and shorter sleeve coping. The abutment teeth that have more alveolar bone support and less mobility receive less tapered and longer sleeve coping. These sleeve copings gain more retention for the CSC prosthesis and lend support to the weaker abutment teeth.
SECONDARY CROWN:
It may be made in type III gold alloy, semi-precious gold alloy or ceramic type metal alloy, with or without acrylic resins or fused porcelain. The secondary crowns are solder connected teeth to each other and to a frame work to which missing teeth and saddle segment are processed. The secondary crowns “telescope” or cover the sleeve copings and serve as removable retainers for the CSC prosthesis.
The secondary crown must exhibit a precise fit on its corresponding steel coping when fully seated. The margins are supragingival and may be further shortened if parallelism is a problem.
FRAME WORK:-
The framework is a major connector to which secondary teeth crowns are solder connected. Denture teeth can be attached to the framework with processed acrylic resin or cemented to pin receptacles with dental cements.
The metal components that join the secondary crowns and saddle segments into one unit may be cast in chrome-cobalt, type III gold alloy, and semi-precious gold alloy at ceramic type metal.
When segments of frame work are cast with secondary crowns they are termed as “interconnection bars”.
The design of frame work is determined by strength, number and position of the abutment teeth available.
Thus, instead of fixed retainer and a separate removable partial denture with various retainers, the CSC prosthesis is the complete entity. A more physiologic linkage results between the tooth support and soft tissues support the CSC remarkable prosthesis, thus eliminating mechanical retainers such as class, precision attachments and stress breakers with their attendant problem.
BIOMECHANICS:
The design of the prosthesis should be such that it is less destructive to the health of already weaker abutment teeth. In order to diminish the retentive torque of abutment teeth, following principles are used.
- Conical taper.
- The slip clutch i.e. clearance for rotation.
- Splinting.
- Shortened lever.
ADVANTAGES:
The CSC prosthesis accomplishes a biologically acceptable linkage between hard and soft tissue support with the following advantages.
- Stress breaking can be physiologically attained.
- The work load can be varied on each abutment tooth depending upon its alveolar bone support and its ability to withstand stress.
- Elimination of solder connectors between abutments. This it has following advantages.
- i) It is more physiologic.
- ii) Kinder to soft tissues.
- iii) Eliminates cementation failure.
- Less stress to stronger abutment tooth then that excreted by solder-connectors to mobile tooth.
- Easier plaque removal.
- Stimulation of papillae or col areas achieved by simple manipulation with round ended bristles.
- The clinical crown to root ratio can be achieved by simple manipulation with rounded ended bristles.
- Maximum force is directed through long axis of the abutment teeth.
- Cross arch splinting is attained when forces are vertically induced thus benefiting the weak abutments. Cross arch torque which often causes cementation failures and periodontal breakdown of weak abutment teeth when fixed prosthesis or rigid retainers for removable prosthesis are used is reduced.
- More biological environment is created around abutment tooth by embodying crown contours designed for each separate abutment tooth.
- Positive gingival coverage is not a problem due to the positive vertical holds offered by the sleeve-coping covered abutment teeth (YALISOVE and DIETZ 1977).
- Secondary crown margins are supragingival can be altered at any time. Mechanical retainers such as clasps, precession attachments, and stress-breakers are eliminated with their attendant problems, thus making the entire prosthesis more physiological.
- Labial and buccal flanges can be removed from abutment teeth thus eliminating contour problems and gingival irritation.
- If and when an abutment tooth is lost it can be added to the crown sleeve coping prosthesis with simple chair side procedure.
RAPPORT:
In addition to an explanation of the risks involved in the therapy, limited prognosis (if such is the case), future modifications \conversion of the prosthesis, and the patient`s responsibility for the success \failure of complex dental prosthesis must be discussed.
CLINICAL PROCEDURES:
PROVISIONAL REMOVABLE PROSTHESIS:
- Should be inserted along with the placement of provisional crowns and splints on the prepared abutment teeth.
- If removable partial denture is present it should be altered\rebased.
PREPARATION OF ABUTMENT TOOTH \ CASTING OF COPING:
Mounted, articulated diagnostic casts are helpful when planning the time plane of proposed occlusal able for severe posterior bite collapse or badly extruded abutment teeth, elective endodontics is necessary to allow for sufficient reduction of the clinical crown of the affected abutment tooth.
Removal of 2mm of tooth structure or more from occlusal or incisal surfaces is required to make room for two thickness of metal. (i.e., of the sleeve coping and secondary crown, plus the cement between sleeve coping and Abutment. A minimum of 3 mm must be removed if ceramometal secondary crowns are used.
The taper of the final preparation is decided prior to starting the preparation and it is dependent on the quantity and quality of alveolar using of the tooth. The degree of taper of the final preparation is inversely proportional to the amount and quality of bone support. Weaker teeth should have more occlusal or incisal reduction and a greater taper of their clinical crowns than strongly supported teeth.
Removal of sufficient tooth structure is mandatory to permit establishment of physiologic contours of secondary crowns.
The ideal type of preparation of on abutment that is to receive sleeve coping is a modified chamfer apical finishing line with a slight bevel beyond the chamfer extending within 0.25 or 0.50mm of the junction of connective tissue to the tooth structure. After the crown preparation, provisional restorations are provided.
Impressions are made and dies are prepared from the casts fabricated. Wax pattern is fabricated for the sleeve coping and casted. The castings are tried and adjusted, the sleeve copings are cemented. When the secondary crowns are clinically acceptable an over-all impression of the arch is made, including edentulous area and the teeth. The framework of the final prosthesis is fabricated over the cast fabricated from the final impression.
TRY-IN OF THE SLEEVE-COPING PROSTHESIS:
After the framework is tried and adjusted in the mouth, the secondary crowns and the framework are assembled by soldering or luting with. The prosthesis is then tried in the patient’s mouth. The secondary crowns and framework during trial insertion should demonstrate the following.
- The assembled prosthesis should be inserted and removed from the coping covered by abutment teeth without noticeable binding of the secondary crown to sleeve coping.
- The framework should not cause discomfort to the patient upon insertion and removal. It should contact the soft tissues accurately and intimately except at the mesh areas to permit the flow of acrylic resin into these areas which creates an interlocking mechanism.
- Framework should not gauge the interdentally papilla and palatal gingival tissues. It should not bind against nor produce torsion of the secondary crowns and once accurate fit is established the palatal framework should stay in place without being held by the operator, otherwise it will not have necessary retentive stability to prevent its dislodgement.
- During the luting of the maxillary secondary crowns to the palatal framework with acrylic, the framework should be held against the palate with sufficient force so as to displace the mucoperiosteum to the full extent of its functional yield.
- The intimate contact of the framework to the palatal tissue is a key to :
- The continuing periodontal health of the maxillary abutment teeth.
- The stability of the prosthesis when the tissues are at rest and the teeth of the opposing jaws are not in contact with the prosthesis. The preservation of maxillary bone and soft tissues for as long as the crown and sleeve-coping prosthesis is in service.
- The technique for luting the mandible framework is different from that of its maxillary counterpart, in that it should be adapted so closely to the secondary crowns that only 0.25 mm of space for solder connection exists.
- If Kennedy’s bar is used it should accurately fit the lingual surface of the anterior teeth to prevent food lodgment, but if a lingual bar is used, it should clear the mucosa by thickness of one sheet of 28-gauge wax. The mandible framework is not held under pressure while being luted to the secondary crowns.
- The assembled prosthesis should exhibit stability when inserted completely and a retentive resistance to dislodgment.
- After this, arrangement of artificial teeth is done and tried in patient’s mouth.
INITIAL INSERTION AND TEMPORARY CEMENTATION:
- The sleeve-copings are filled with a mixture of petrolatum paste and ZnO as a pressure indicator.
- The posterior palatal extension must be checked. Careful adjustment of all acrylic tissue bearing areas must be made until complete palatal seating is accomplished.
- When the prosthesis fits comfortably preliminary occlusal adjustment should be made so that the prosthesis remains fairly stable as the patient goes through various mandible excursive movements.
FINAL CEMENTATION OF THE PROSTHESIS:
Performed after 3-4 days of trial cementation and the objectives include:
- Each sleeve-coping should be completely seated on its corresponding abutment tooth.
- The marginal fit of each sleeve-coping should be accurate and non-abusive to the sulcular tissue.
- The tooth-to-tooth relationship of the secondary crown should be accurate and correct. There should be absolute stability of the prosthesis when force is applied through the long axis of each secondary crown.
FINAL EXAMINATION:
- The patient should be re-examined 2-3 weeks to ensure that there is no impingement of the prosthesis into the soft tissues along with the comfort of the patient.
- The sleeve-coping should fit the abutment teeth accurately.
- There must be an intimate functional fit of the secondary crowns to the sleeve-copings.
- Gingival margins of the secondary crowns must not extend sub-gingivally.
- There must be an accurate fit of the metal framework to the palate or to the mandible ridges.
- An accurate solder transfer must be obtained when secondary crowns are luted to the framework intra-orally.
- The solder assemblage of the prosthesis must exhibit complete stability.
- When functional impressions of edentulous areas are made, the secondary crowns must be fully seated upon the sleeve-copings.
- If the prosthesis bounces back, disclosing paste should be used on tissue surfaces\ to expose excessive acrylic resin causing impingement.
The CSC prosthesis differs from the tooth-supported complete denture in the following ways.
- The crown and sleeve coping prosthesis use abutment teeth with longer clinical crowns then these used for implant overdenture & thus exhibits more frictional retention.
- The additional frictional retention furnishes greater stability for the crown and sleeve prosthesis.
- The vertical dimension of occlusion and centric occlusal hold areas are better preserved with metal or ceremometal occlusal or incisal surfaces in comparison to with hallowed out acrylic denture teeth.
- Plague control is much easier because of absence of buccal & labial flanges.
- By salvaging more teeth and using them as abutments, CSC prosthesis preserves alveolar bone & denture base tissue for longer time.
- As this prosthesis resembles more to fixed prosthesis then complete denture, it improves masticatory efficiency & provides greater psychic satisfaction associated with retention of natural teeth.
COMPLICATIONS WITH OVERDENTURE THERAPY:
Long term studies of implant overdenture sequela are relatively sparse, but most agree that periodontal disease and caries are the two major problems. Of the two, Periodontal disease would appear to be a more widespread and potentially dangerous problem. This is demonstrated by RIETZ and his associates in their studies.
PERIODONTAL PROBLEMS:
The periodontal problems may range from gingival recession, simple marginal gingivitis to advanced destruction of bone as in the case of severe periodontitis which could lead to the loss of teeth. In REITZ and associates study (1977), 50 patients with 131 abutment teeth and 59 over dentures were evaluated in 1974. The time from insertion to the time of survey ranged from 6-47 months, the mean being 19.2 months. Only one of the 50 patients lost support of the tooth. Interestingly even over dentures rated as “failing” functioned satisfactorily for the patients. Another complication seen with poor oral hygiene and inadequate adaptation of the denture base is the “edematous hyperplasic gingivae”.
CARIES:
The patient must be informed of the possibility of dental decay, which can seriously affect th remaining natural teeth. If copings are necessary, due to extensive caries, roots weakened by old restorations, a high caries index and attachment cases it is advisable to wait for 3-6 months before making the copings. RIETZ and his associates (1977) survey, reported a caries incidence of 16% in the first survey and 20.6 % in the second.
LACK OF REGULAR EXAMINATIONS:
The need for regular recall examinations is probably more important for the overdenture implant patient than in any other phase of prosthodontics. Most overdenture implant patients have lost their teeth due to neglect. A common sequela that have to be checked regularly is the settling of the denture bases which causes excessive pressure upon the gingival tissues of the abutment teeth. The use of pressure indicating paste will easily identify these areas and correction can be easily made. If this simple procedure is not done, continuous pressure can cause atrophy and loss of attached gingivae.
CHANGING RELATIONSHIPS OF THE DENTURE BASE TO THE TEETH AND RIDGE:
The base of the denture should be related to the teeth and ridge tissues so that the support is simultaneous and even. Under functional loading the resiliency of the average tooth is 0.1 mm, and the alveolar ridge is 0.4-2 mm. (STEGIER and BIOTEL). A reline technique for abutment teeth is needed to achieve even support.
INCORRECT ABUTMENT TOOTH HEIGHT :
If an abutment tooth is insufficiently reduced, mobility and discomfort may be evident. This is probably due to the unfavorable crown-root ratio and can be easily corrected, especially when a gold coping is not used.
On the other hand over-reduction of the abutment teeth results in proliferation of the soft tissue. Also, the overdenture implant will have less stability, incurring a vicious cycle of more movement and further tissue irritation and proliferation. This condition is best corrected with gold copings.
BREAKAGE:
Denture base breakage is a potential problem with the overdentures implant as their design is inherently weak because indentations of the denture base are required by the abutments. Breakage is almost completely controllable by using all resin teeth and high impact material for the denture base. If needed, cast inserts or bases will almost always prevent breakage.
WEAR OF THE DENTURE BASE AND\OR ABUTMENT TEETH:
This is especially common if the opposing occlusion is another overdenture implant, a removable or fixed partial denture, or natural teeth. Wear can be avoided by making gold coping and using metal occlusal on the overdenture implant. If the wear has already occurred, the denture base can be corrected with an abutment reline. The abutment tooth can be refilled with a new alloy or gold coping can be fabricated followed by abutment reline.
ปั้มไลค์
27 Jul 2020Like!! Thank you for publishing this awesome article.
Sumit Vasant Duryodhan
6 Aug 2020Mam, thank you so so so much for all this..
Elenor Walby
25 Sep 2020This wonderful and very well written article reminded me of when I had big problems with teeth, cavities
and pain, yellow and ugly teeth, then I found a simple way to
rebuild my teeth and gums and get rid of tooth decay. (maybe it will help someone):
https://bit.ly/2ZV061N Thanks! Keep doing a great job!
Cukrzyca.XMC.pl
1 Mar 2021I have study a couple of the articles on your site since yesterday, and I truly like your way of blogging. I tag it to my bookmark web site list and will be checking back soon. Please check out my web site also and let me know what you think.