
Denture stomatitis is a direct sequela of wearing dentures. It is mainly due to wearing complete or partial dentures at night or not maintaining oral hygiene. Extooth presents you with the best cheat sheet for the best oral hygiene to prevent any oral disease.
The primary cause of any disease is an infection. You can prevent infection thereby preventing Denture Stomatitis by making your mouth and denture clean. I, being a denture specialist has been frequently asked by seniors how to clean dentures at home.
It occurs in 50% of the people wearing complete or partial dentures.
It is the pathological reaction of the denture bearing mucosa to denture causing inflammation of the tissues beneath the dentures.
Synonyms for Denture Stomatitis
Denture Sore Mouth,
Inflammatory papillary hyperplasia,
chronic atrophic candidiasis
Prevalence of Denture Stomatitis
It occurs among 50 % of denture wearers.

Classification of Denture Stomatitis
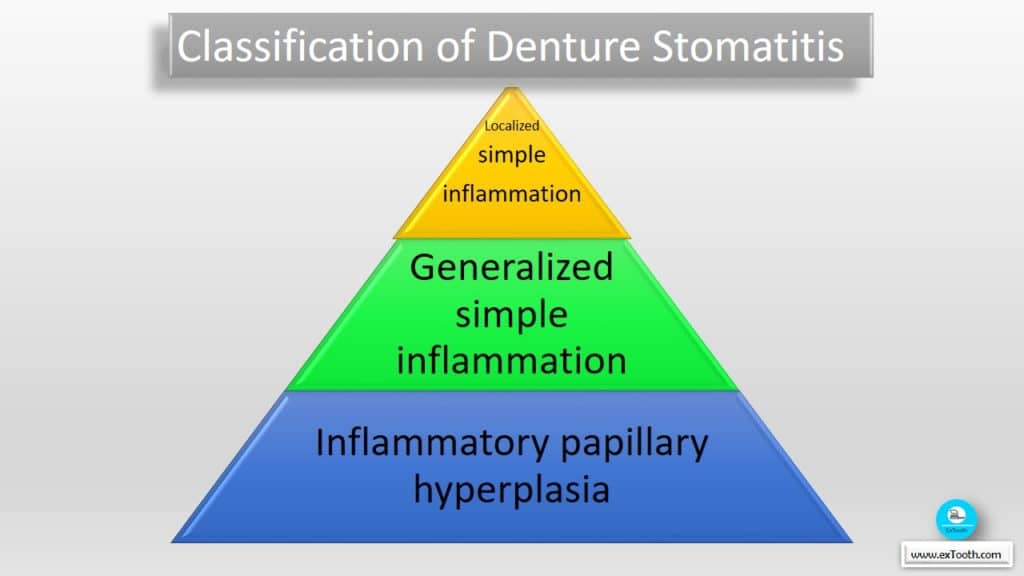
Newton has classified it into 3 types-
1) Type-1: a localized simple inflammation or pinpoint hyperemia
2) Type-2: an erythematous or generalized simple type presenting a more diffused erythema involving a part of the palate or entire denture bearing mucosa.
3) Type-3: Agranular type (inflammatory papillary hyperplasia) commonly involving the central part of the palate and alveolar ridges. Type 3 is often seen with type 1 or type 2
Causes of Denture Stomatitis
1. Candida infection
2. Bacterial inflammation
3. Mechanical irritation or allergy
Type 1 is trauma-induced.
Types 2 & 3 by microbial plaque accumulation on fitting surface & underlying mucosa Candida associated will be often spread leading to angular cheilitis or glossitis.
Diagnosis of Candida associated Denture Stomatitis
Candida associated denture stomatitis is confirmed by finding of mycelia or Pseudohypphae in the culture and\ >50 colonies of Candida species . Usually, yeasts are recovered in higher numbers from fitting surfaces than from corresponding areas of palatal mucosa. This indicates that Candida residing on the fitting surface of denture is a primary source of infection.
Pre disposing factors to Candida associated denture stomatitis
Factors predisposing to Candida associated denture stomatitis are
Systemic factors
1. Old age
2. Diabetes mellitus
3. Nutritional deficiencies (Iron, folate, vit B12)
4. Malignancies (Acute leukemeias, agranulocytosis)
5. Immune defects
6. Corticosteroids, immunosuppressive drugs.
Local factors
1. Dentures (Changes in environmental conditions, trauma, denture usage, denture cleanliness)
2. Xerostomia (Sjogren syndrome, irradiation drug therapy)
3. high carbohydrate diet
5. smoking tobacco
Presence of denture in the oral cavity is one of the direct predisposing factors for Candida associated stomatitis.
It is prevalent in patients who are wearing their dentures both day and night.
Leaving out dentures will cause the inflammation to disappear, it is likely that bacteria which constitute the major part of microorganisms of denture plaque, also are involved in the infection. Furthermore, healing of lesions often is seen after initiating meticulous oral & denture hygiene.
Management and preventive measures of Denture Stomatitis
1. Correction of an ill-fitting denture
· Any ill-fitting denture has to be corrected & relined if necessary.
SHORT-TERM SOFT LINERS (TISSUE CONDITIONERS)
Tissue conditioners remain soft for days to weeks. For sufficient cushioning, tissue conditioners should be substituted with newly mix every 2 to 3 days. This procedure is maintained until the full rehabilitation of tissues.
INDICATIONS:
Treatment and conditioning of abused/ irritated denture supporting tissues prior to impression making for new dentures
COMPOSITION
Available as:
• Powder/ liquid
• Preformed sheets of acrylic gels
Powder-
polymer,a polyethylmethacrylate(PEMA) or its copolymers
Liquid –Mixture of ethyl alcohol (solvent) & aromatic ester- dibutyl phthalate (plasticizer)
Trade names of tissue conditioners: viscogel, coe comfort
MECHANISM OF GELATION
· Gelation of tissue conditioners is a physical process (devoid of any chemical reaction or any monomeric substances that could cause tissue irritation).
· Upon mixing the powder and liquid, the alcohol/ Plasticizer mix diffuses into the swellable acrylic beads. Gelation involves the entanglement of outer polymer chains of swollen beads, resulting in a tacky set gel with high cohesive properties.
MECHANISM OF ACTION
• Tissue conditioners show a combination of both viscous fluid and elastic solid behavior
• The viscous course provides conditioning gel to inflamed/ irritated mucosa, enhancing the fit of the denture
• While chewing, the material exhibits a time-dependent elastic response that permits it to recoup initial deformation, grasping impact forces and cushioning the underlying tissues
DISADVANTAGES
• Temporary variety of tissue conditioners derives from the fact that both the alcohol and Plasticizer leach out and are partly replenished with water
• The material thus sets within a considerably little time
• The material becomes vulnerable to surface deterioration, contamination, and fouling by microorganisms.
TECHNIQUE IN THE USE OF A TISSUE CONDITIONER
a. Pre-requisites for the use of this material are as follows:
The dentures have adequate coverage of the bearing area, a good centric relation, adequate occlusal vertical dimension, no gross interferences in eccentric jaw positions or that the dentures could have the above-mentioned prerequisites incorporated with minimal adjustments. These are of paramount importance. Since most of the discomfort from dentures can be attributed to poor occlusion.
b. Preparation of the denture:
Remove from the denture base all undercuts and some of the area immediately on the ridge to a depth of 1mm or more. Retain borders or flanges and the hard palatal area in the maxillary denture as vertical stops in a seating or placing it on the ridge.
c. Preparation and placement of the tissue conditioner in the mouth:
The material to be used is a three-component system, the polymer(powder) the monomer (liquid) and a liquid plasticize (Flow Control).
Flow-control is added to the liquid monomer and mixed prior to mixing it with the polymer. This differs from what the manufacturer recommends. In a glass, jar mixing is done by slowly adding the powder to the liquid and stirred continuously until the desired amount of it is incorporated in the mixture. Material thickness by virtue of its own reaction, while the material is still creamy and runny, it is poured into the denture and made certain that the entire area of the denture base is covered. When material ceases to flow readily denture is inserted in the patient’s mouth. Slowly but firmly denture is carried to place. Opposing dentition is used as a guide to centric relation. Dentures are held in this position at the desired occlusal vertical dimension for 3 minutes.
Following this patient is instructed to move his or her lips and cheek to border mold the material. Excess loose material in the mouth is removed. After the material is set, the excess is trimmed by sharp knife scalpel or scissor. Denture inspected for pressure areas and then relieved. Later small amounts of material are added and the denture is returned into the patient’s mouth for contouring. Once an even thickness of 1mm or better of conditioning material is satisfied, the sharp cut edges, as well as all the material surfaces, is covered with a small amount of the “flow control” to allow the conditioner to continue to flow and contour itself as the tissue recover. Also, this will enable the sharp corners to be rounded and become smoother and lustrous as the patient uses the denture.
Dentures are returned to the mouth to check for comfort and the patient is instructed with the care of the denture. The patient is told to return the following day for inspection and correction of pressure areas and this procedure is repeated every 3-4days until the traumatized and irritated tissues have fully recovered. The patient is told not to eat hard-to-chew foods for the first 8 hours following the application of the material. Since this may have a tendency to squeeze the conditioner out of shape, destroying what has been previously accomplished.
2. Efficient plaque control
· Patients should be instructed to remove dentures after the meals & scrub them vigorously with soap. Know how to make your denture crystal white, click here.
· Mucosa should be kept clean massaged with a soft toothbrush
· Patients with recurring infections should be asked to leave their dentures outside the mouth at night. & leave them outside in the air. This reduces microbial colonization.
· A new denture has to be provided only if mucosa has healed and the pt maintains good oral hygiene.
3. Antifungal therapy
· Can be instituted after elective verification of Candida infection using a palatal smear.
· A therapeutic dose of one nystatin tablet taken thrice daily for 10-14days
· Other drugs such as amphotericin B, miconazole or clotrimazole should be preferred to systemic therapy with ketoconazole or fluconazole as these produce resistance to candida species.
· this combination may be instituted for 4 weeks
· if lozenges are prescribed, patient is advised to takeout dentures during sucking
· Patient should be instructed in meticulous oral & denture hygiene; the patient should be told to wear the denture as seldom as possible & to keep them dry or in a disinfectant solution of 0.2-2 % CHX during the night.
4. Surgical correction
· Surgical elimination of deep crypts in type III cases is a prerequisite for effective oral hygiene. This can be done using cryosurgery.
Leave a comment if you have seen a patient or suffered from Denture Stomatitis.
Pooja
11 Jan 2020Thanks for knowledge
Sunitha S
15 Jan 2020Informative post. Thanks for sharing.
Martin Litano
14 May 2020I am glad that I found this article well documented and very informative.
I want to share how I treated Yeast and Candida Infection, maybe it will be
useful to someone: https://bit.ly/3cq12iO
Thank you and keep going, you do a great job!!
bedava
9 Feb 2021Awesome write-up. I am a normal visitor of your blog and appreciate you taking the time to maintain the excellent site. I will be a frequent visitor for a really long time. Nanni Padget Clarette
erotik
13 Feb 2021Great blog here! Also your site loads up very fast! What web host are you using? Can I get your affiliate link to your host? I wish my web site loaded up as quickly as yours lol Oralla Stefan Stephine
erotik
17 Feb 2021Everything is very open with a really clear explanation of the issues. It was really informative. Your website is very helpful. Many thanks for sharing! Anatola Harp Jabe