NUTRITION AND ORAL HEALTH
Let’s discuss the effect of nutrition on oral health.
Nutrition is processed by which we take and utilize foods.
Diet is the measure of consumption of food by us.
Nutritional Status: this term refers to the condition of health as influenced by the utilization of nutrients.
Vitamins are the group of substances that are essential for the normal functioning of metabolism in the body.
They can not usually be synthesized in the body, but they occur naturally in some foods.
BMR: The minimum energy return needed for the maintenance of cellular metabolism when the body is in the basal condition is called the basal metabolic rate.
Balanced diet – Nutrition and Oral health
A stable diet is one that contains all the food constituents in proper balance to meet the energy and nutritional demands of our body.
The relationship between protein, fat, and carbohydrates in a balanced diet should approximately be 1:1:4, respectively.
The insufficiency of essential nutrients can result from poor diet
Malabsorption from the gut
Factors limiting blood transport or uptake in the mucosa
Low storage
Increased Metabolic demand
Excessive loss from the body.
VITAMINS
Vitamins: are classified into two types.
Fat-soluble vitamins – A, D, E, K
Water-soluble vitamins – C and B complex
Vitamin A : (Retinol) –(Anti-infective vitamin )

Vitamin A is obtained from animal tissues only.
The richest sources are sea fish liver oils, cod liver oil, shark liver oil, butter egg yolk are other good examples.
Beta – Carotenes and similar compounds are collectively called as provitamins
Beta – Carotenes are found in green plants and leafy vegetables.
Vit A is the provitamin and retinoic and is the active constituent. The term ‘tretinoin’ means the retinoic acid is the active form of Vit A in tissues. Synthetic analogs of Vit A are known as retinoids.
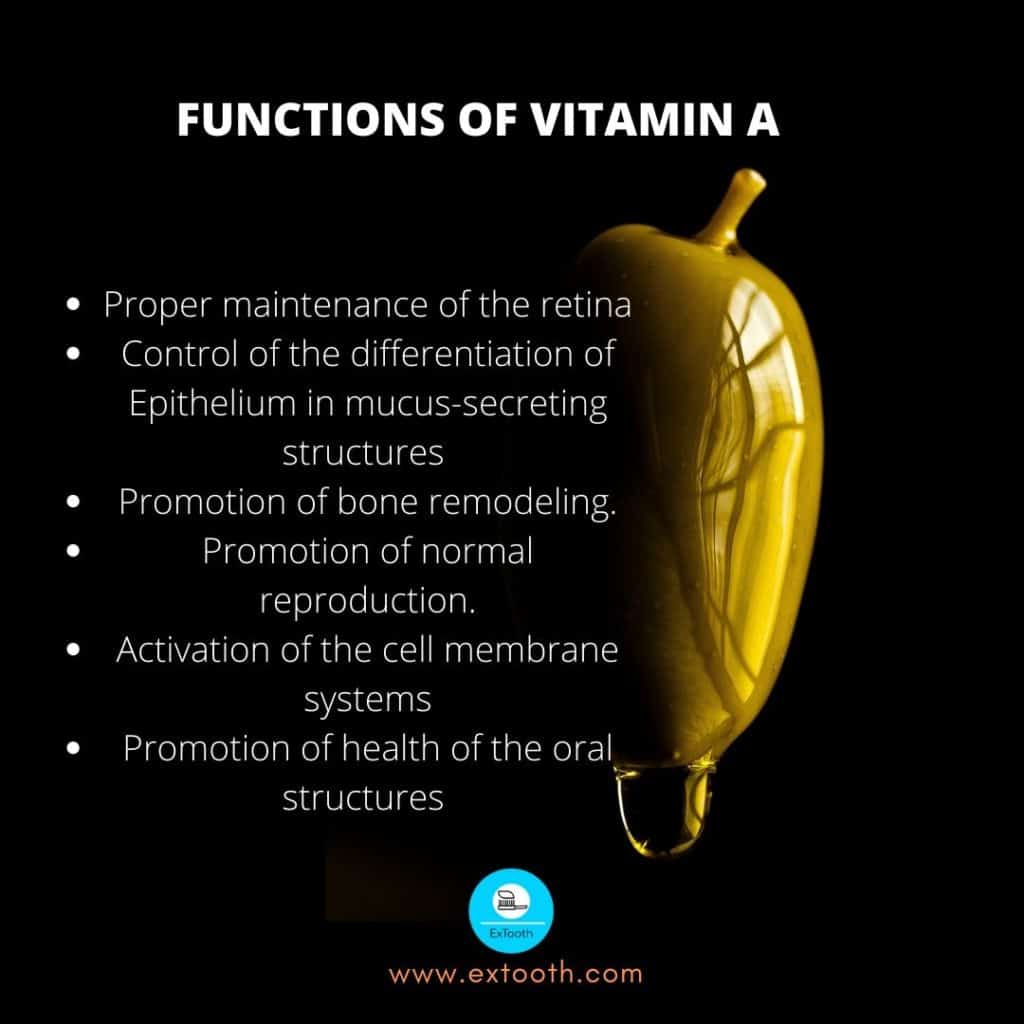
Vitamin A has the following functions :
- Proper maintenance of the retina
- Control of the differentiation of Epithelium in mucus-secreting structures such as the salivary glands, the nose, and the throat.
- Promotion of bone remodeling.
- Promotion of normal reproduction.
- Activation of the cell membrane systems such as endoplasmic reticulum and plasma membrane
- Promotion of health of the oral structures – The teeth, periodontium, and oral mucous membrane.
Maintenance of Epithelial cells and Tissues
Influences genes because vitamin A affects the differentiation and proliferation of cells. The main function of Vitamin A is to maintain the health of epithelial cells of the skin and membranes.
The epithelial cells are the first line of defense against invading bacteria and other microorganisms, but without Vit A, they will undergo degenerative changes. Vitamin A is responsible for the production of glycoprotein, the substance from which mucus is made. In the absence of Vitamin A, the mucous secreting cells will degenerate and produce keratin instead of mucus.
Without Vitamin A, the scleral and corneal epithelia of the eye become keratinized. The regular mucosal surfaces of the conjunctiva become dry and granular, and severe secondary infection may occur. When keratin debris piles in whitish plaques, it is called Bitot’s Spots.
The keratinization and thickening of the corneal epithelium produce xeropthalmia, which leads to weakened vision. There also may be weakening of the cornea, leading to deformation and destruction. This is known as keratomalacia.
In the absence of Vitamin A, the normal columnar ciliary epithelium of the nose, the nasopharynx, and the rest of the respiratory tract is replaced by non-ciliated stratified squamous epithelium. This loss of cilia reduces the normal defensive/function of the mucosa.
Follicular hyperkeratosis – A rough, sandpaper-like skin and numerous papules caused by the closing of the hair shafts and the sebaceous gland ducts is a characteristic response to deficiency of vitamin A.
Promotion of bone remodeling
In young animals, experimentally produced Vit. A deficiency is accompanied by the end of bone growth. The defect of bone growth is thought to result from a failure in the normal conversion of osteoblasts to osteoclasts, which causes a breakdown of bone during the process of bone remodeling.
Activation of cell membranes
Vitamin A ensures the normal structure and function of biological membranes of cells. In severe Vitamin A deficiency, abnormalities of both RNA metabolism and protein synthesis have been reported.
Consequences of Vitamin A deficiency on oral structures – Nutrition and oral health
Nutrition and oral health (VITAMIN A)
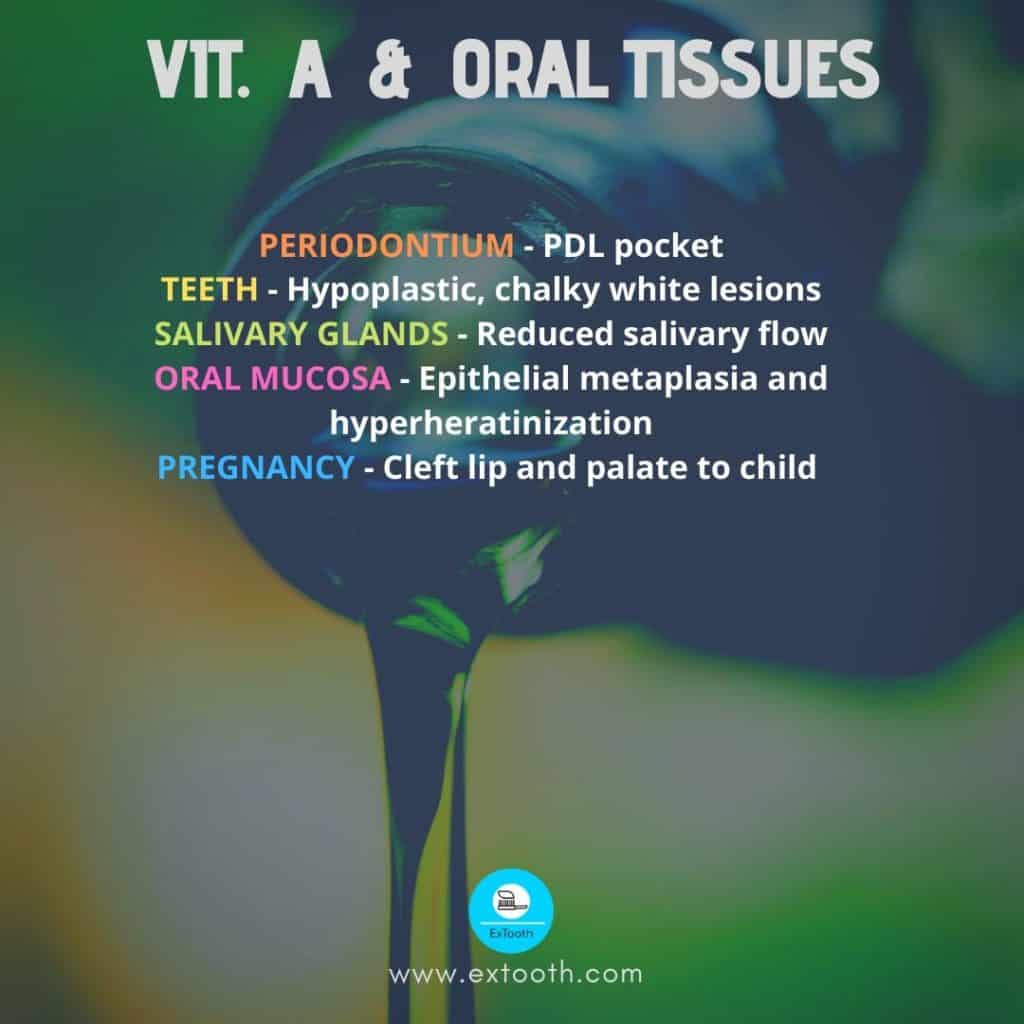
- In the periodontium – Nutrition and oral health
In experimented animals, Vit. A deficiency produces hyperkeratosis and hyperplasia and gingival tissues. There is a tendency to a periodontal pocket formation as a result of the proliferation of basal cells of the gingival epithelium and decreases cellular infiltrate of the lamina propria. When trauma or irritation is superimposed on this conditioned deficiency, severe pocket formation will occur as a result of increased repair activity.
2. Nutrition and oral health – effect of Vit. A on the teeth
In Vitamin A deficiency, ameloblasts fail to differentiate properly; therefore, they produce hypoplastic and chalky white lesions. Also, diseases of the labial and lingual odontoblasts occur, creating thick, normal labial dentin with inter globular spaces and a thin, tubular lingual dentin. Crowding of teeth and stunting and thickening of the tooth roots can also be seen in Vitamin A deficient animals.
In individuals, the teeth are limited receptive to this deficiency. There is no absolute correlation between vitamin A deficiency and dental caries or enamel hypoplasia in humans, probably because the deficiency has to be very serious, which rarely if ever, occurs.
3. In the salivary glands – Nutrition and oral health
The atrophy of the Salivary glands resulting from a Vit A deficiency will reduce salivary flow and consequently increase caries.
4. In the oral mucous membranes – Nutrition and oral health
Because Vitamin A deficiency is associated with epithelium metaplasia and hyperkeratinization, it has been proposed that oral leukoplakia might respond to larger doses of Vitamin A. This type of therapy has not yet received wide acceptance because its efficacy has not been clearly understood.
Cleft lip and palate – during early development, both deficiency and a high dose of vitamin A have been reported to produce cleft lip and palate in a child.
Recommended dietary allowance
For adult, man is 5000 IU
Female is 4000 IU
Toxicity
Too much of anything is bad!
Hypervitaminosis A
In adults, hypervitaminosis A has occurred in individuals who are given 100,000 to 150,000 IU as a treatment for acne. Anorexia, irritability, loss of weight, tenderness over the long bones, and enlarged spleen and liver are special findings. Hypercarotinemia (Serum carotene level above 250 ug/ml) will give yellow-orange discoloration of the skin and oral mucosa. It may arise from excessive intake of carrots.
VITAMIN – D
It is one of the fat-soluble vitamins, also known as a prohormone.
Chemistry
Several types of Vitamin D are known, of them Vit. D2 and D3 are the most important. The precursor of Vit. D3 is 7-dehydrocholesterol. 7-Dehydrocholesterol normally occurs in the skin. Chemically, it is a steroid and contains a CPP ring. When exposed to ultraviolet rays, it is converted to D3. Vit D3 is also called “irradiated dehydrocholesterol.” Vit D2 is obtained from ergosterol, which is a plant sterol. Ergosterol, when irradiated by ultraviolet rays, is converted into Vit D2. Vit D3 and D2 also known as cholecalciferol and ergocalciferol, respectively. Both are known by generic name Vit.D.
Source Fish liver oils, milk, egg, yolk
Infants and children -5 ugms/day
Adults- 2.5 ugms / day
Locating mothers and pregnants -10 ugms/day
Functions
Vit. D is a prohormone. In the body, it is converted into a steroid hormone
1, 25 dihydroxycholecalciferol, to its active part.
Vit. D3 is formed from 7-dehydrocholesterol and is then bound by a specific globulin called D binding protein. The protein-bound Vit. D3 circulates in the blood and reaches the liver where it is hydroxylated at C-25 position to form 25 hydroxycholecalciferol. This compound then reaches the kidney where it is further hydroxylated so that 1,25 dihydroxycholecalciferol is formed.
Small intestine and bone are the principal target organs of 1,25 dihydroxycholecalciferol. In the intestine, 1,25 dihydroxycholecalciferol causes increases absorption of food calcium. The active absorption of calcium is increased.
On the bone, it increases the calcification. This is chiefly the result of increased availability of calcium as a result of increased calcium absorption from the intestine. 1,25 dihydroxycholecalciferol is capable of causing increased calcium deposition by acting on bone cells. Apart from the small intestine and bone, the kidney is another target organ. 1, 25 dihydroxycholecalciferol causes increases reabsorption of calcium from the distal renal tubules.
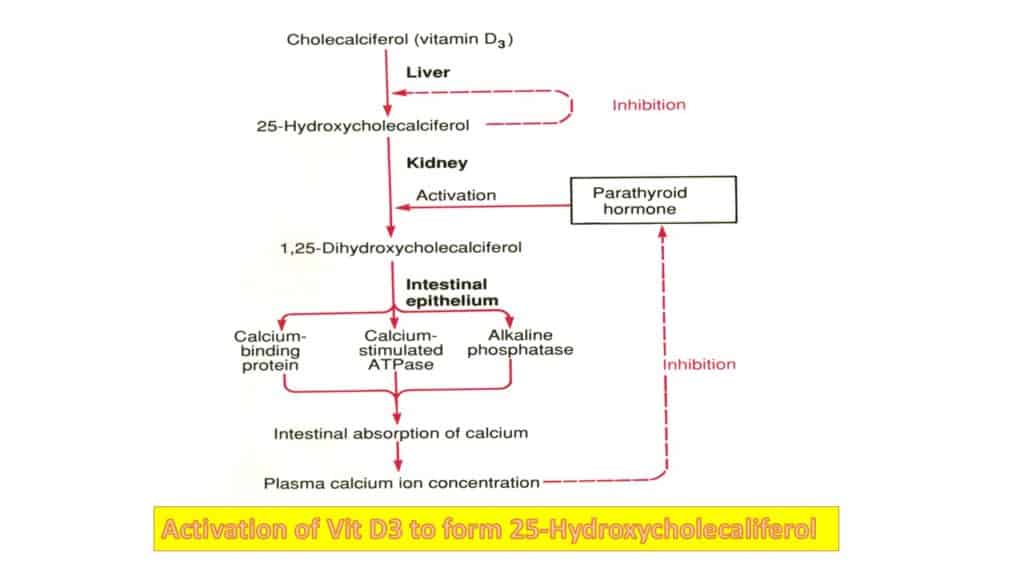
The active principle 1, 25 dihydroxycholecalciferol acts as a typical steroid hormone. Thus, via blood, it reaches the intestinal epithelium. It enters the inside of the epithelial cell and ultimately causes more RNA synthesis. These RNA cause more synthesis of a specific protein that acts as a carrier protein; this specific (carrier) protein binds with the calcium of the intestinal lumen (food calcium) and transports the calcium into the interior of the lining epithelial cell. From the cytoplasm of this cell, the calcium is finally removed and transferred to the venous blood.
Regulation of formation of 1, 25 dihydroxycholecalciferol
Presuming there is no deficiency of vit.D in the body the formation of active principle is regulated as follows :
If there is a fall of serum Ca++ Level the PTH is secreted in increased quantity, PTH acts on the kidney so that 1-hydroxylase, which hydroxylates the 25 cholecalciferol is activated and 1, 25 dihydroxycholecalciferol is formed. If the serum Ca++ is high, PTH secretion is minimum, and hydroxylation does not occur.
APPLIED PHYSIOLOGY
Rickets
This happens in kids who are not exposed to sunlight and whose diet is deficient in Vit. D. The changes are as follows :
In the bones, calcium content is below, and bones convert consequently soft. Such bones bend when they carry weight as in femur and tibia. The means of ossification in cartilaginous bone is delayed. Usually, cartilage is first calcified. Then removed, and new bones are deposited. In rickets, the calcification of the cartilage is poor, the cartilage cells proceed to proliferate, and the shaft becomes broad and irregular.
Osteomalacia
If there is a lack of Vit. D in adult life, the condition is called osteomalacia. It is equivalent to rickets in an adult’s life. The biochemical test that features to a judgment of Vit D deficiency is an elevated serum alkaline phosphates.
Enamel hypoplasia
The earliest dental differences observed when vit.D deficiency occurs during tooth development, and calcification is hypoplasia. As a result of lack of Vitamin D, the enamel calcifies poorly and may, in some areas, fail to form. In the dentin, spaces that represent the uncalcified dentin matrix occurs. The appearance of a calciotraumatic line in the dentin is the earliest sign of an acute deficiency of Vit D.
There have been various attempts to improve the relationship between adequate intake of Vit D and reduced caries incidence, but this has not been clearly proved.
Vitamin E (Anti-sterility Vitamin)
The most biologically dynamic form is alpha-tocopherol. Vitamin E is absorbed adequately in the presence of fat. States that intervene with fat absorption, such as biliary tract diseases, pancreatic insufficiency, and excessive mineral oil ingestion, decrease the amount of Vitamin E absorbed.
Function
Vitamin E works as a natural antioxidant to restrict free radical chain reactions and to shield body cells from lipid peroxidation and final damage. Cell membranes, which are chief in polyunsaturated lipids, are the primary sites of destruction. Thus the role of Vit. E is to make cell membranes more stable and thus save the cell wall constituents, including those of RBC from damage.
Because of Vit. E is an antioxidant, and it prevents fats from becoming bad.
Vit-E deficiency
Clinical findings: Vit E deficiency is rare in human beings. If a deficiency is present, it is due to congenital or malabsorption disease with results in hemolysis leading to anemia.
Vit. E deficiency may cause impaired neuromuscular function.
Oral Findings in Rats
Vitamin E is essential for maintaining the integrity of the enamel in the rodent incisor. A deficiency of Vitamin E will cause disarrangement of ameloblasts, and the rodent incisors become chalky white.
RDA = 10-20 IU where /IU = 1mg of dl alpha – tocopheryl acetate.

Myths
There are no cosmetic benefits from the application of Vitamin E to the skin in order to remove wrinkles or heal blemishes. The only value of Vitamin E on the skin is from the lubrication action of the oily medium.
The claim that Vit. E prevents cancer and improves activity has not been proved.
Toxicity
Vit. E in larger doses may increase the time required for blood coagulation. The most common signs and symptoms of toxicity are headaches, fatigue, temporary nausea, weakness, diarrhea, blurred vision.
Vitamin – K
Vitamin k is a Fat soluble vitamin
Three types
K1 – K1 group occurs in green plants
K2 – K2 group is produced by the bacterial synthesis in the intestine.
K3 – Synthetic form of the vitamin known as menadione.
It is estimated that appropriate 50% of the daily requirements are derived from a plant source, and the rest is from bacterial synthesis.
Function
The primary function of Vit. K is to catalyze the synthesis of a blood clotting factor prothrombin, by the liver.
Vit. K is essential for the production of other clotting factors like
Factor VII – proconvertin
Factor – IX – Christmas factor
Factor – X – Stuart factor
In the absence of these factors, a prothrombin deficiency develops, and blood clotting is greatly prolonged.
An important therapeutic use of Vitamin K is an antidote to the anticoagulant drug.
Vit. K and Periodontal disease
Vit K compounds have been found to be required for the growth of Bacteroides melaninogenious, an organism widely associated with PDL disease.
It is speculated that a suitable antimetabolite of Vit. K might interfere with the growth of this organism and, consequently, prevent the occurrence of PDL disease.
RDA – 70- 140 ug for adults
Usually, the bacteria in the intestine and the green leafy vegetables in the diet provide ample amounts of Vit.k.
Lettuce, spinach, cauliflower, and cabbage are excellent sources.
WATER – SOLUBLE VITAMINS
- Vit. B complex
- Vit. C
- Vitamin B complex;
- Vit. B1 – Thiamine
- Vit. B2 – Riboflavin
- Vit. B6 – Pyridoxine
- Vit. B12 – Cobalamin
- Niacin
- Biotin
- Pantothenic acid
- Folic acid
Different vitamins have been discovered and classified as belonging to the B complex group. On a functional basis, Vit. B complex is subdivided into
- Those vitamins that primarily release energy from CHO fats, Example
: Thiamin, Niacin, riboflavin, Pantothenic acid, biotin. - Those that catalyzes the formation of RBC. Example: Folic acid, Vit. B12.
- The vitamin that is important in protein and a metabolism; Vit.B6.
- The vitamin-like compounds.
Thiamine (B1)
Thiamine, as thiamine pyrophosphate is an important coenzyme in energy metabolism. It acts as a coenzyme in the production of ribose, the sugar needed by all cells for the formation of RNA, which helps produce protein and DNA, the basic substance of genes. Thiamine is needed for the metabolism of CHO, proteins, and fats. Thiamin has got a specific role in neuro-physiology also.
Deficiency
Thiamine deficiency is called beriberi. It affects CVS, muscular, and nervous systems principally.
Beriberi can be separated into three forms
- Wet * Dry * Infantile
In wet beriberi: edema, Cardiac disturbances such as enlarged heart, systolic murmur, dyspnea. Rapid pulse, irregular pulse, distended neck veins.
In dry beriberi: Paresthesia and numbness of feet cramps in the legs.
In infantile beriberi: dyspnea, cyanosis, and Cardiac failure
In the alcoholic, a severe thiamin deficiency may lead to WERNICKE’S syndrome with is characterized by confusion, paralysis of eye muscles, and loss of memory.
Peculiar gait and wrist drop are seen in advanced cases. The possible oral manifestations of thiamin deficiency have increased the sensitivity of the oral mucosa, burning tongue, loss of diminution of taste.
Diagnostic lab findings
The concentration of pyruvate in the blood is increased so that the ratio of lactic acid to pyruvic acid becomes abnormal. The measurements of transketolase enzyme activity in erythrocytes is a useful test in the diagnosis of thiamin deficiency.
RDA: 1 mg. Thiamin/day
Food sources; cereals, meat, legumes.
Riboflavin (B2)
Riboflavin is an electron transfer vitamin participating in the exchange of oxygen and hydrogen between plasma and tissue cells. In addition to taking part in the formation of ATP, riboflavin assists in the metabolism of CHO, proteins, and fats.
B2 is found in leafy, vegetables, meat, milk, fish.
Deficiency of Vit B2 is commonly dietary, seen especially in alcoholics, and leads to seborrhea dermatitis, corneal vascularisation, and anemia.
Oral manifestations include
- Angular stomatitis
- Glossitis
- Oral ulcerations
Vitamin (B6) pyridoxine
It is found in meat, and vegetables are involved in the formation of pyridoxal phosphate and pyridoxamine phosphate, coenzymes in amino acid metabolism. B6 aids in the conversion of tryptophan to niacin and metabolism of unsaturated fatty acids. It aids in the normal functioning of the nervous system and the synthesis of Hb and RBC.
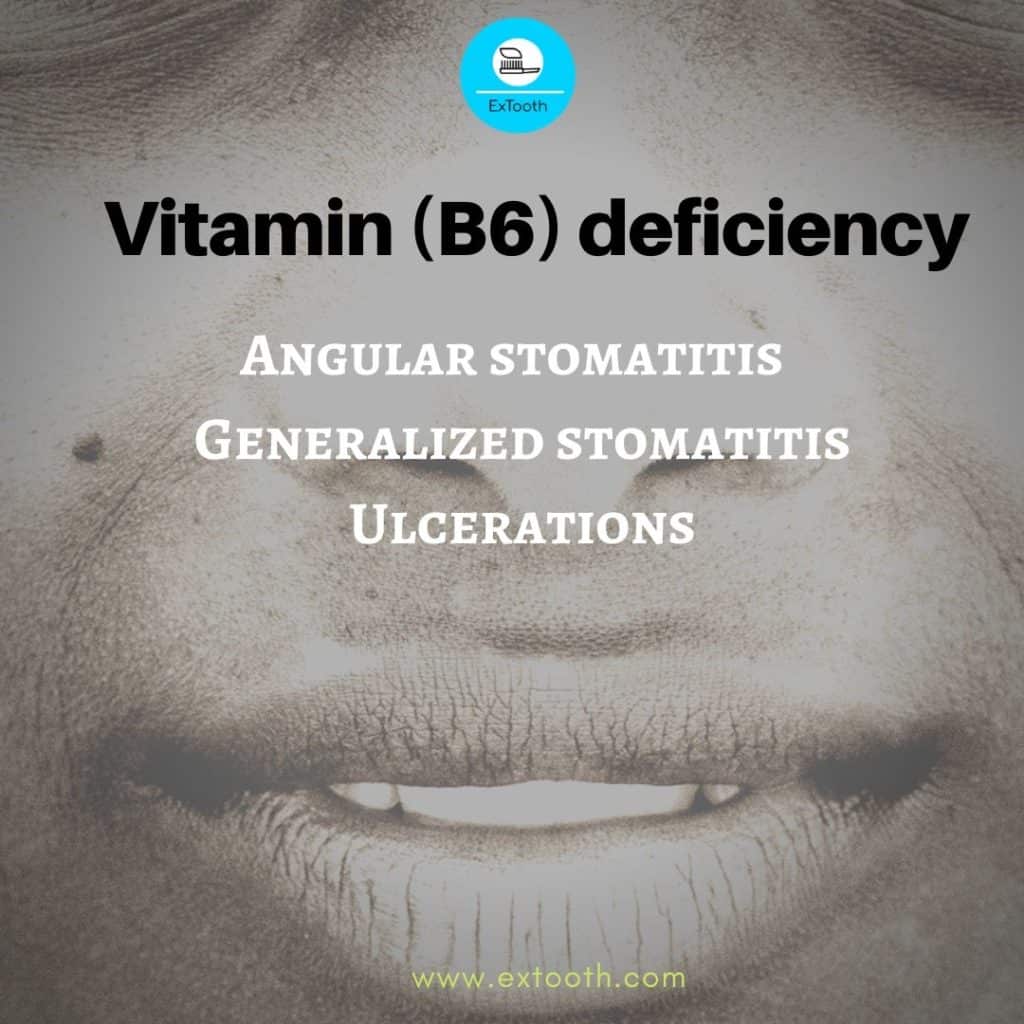
Deficiency
Deficiency is particularly found in alcoholism, pregnancy, and the use of some drugs (isoniazid) and leads to dermatitis, peripheral neuropathy.
Oral manifestations include
- Angular stomatitis
- Generalized stomatitis
- Ulcerations
Pantothenic acid
Pantothenic acid is needed for the synthesis of coenzyme A, necessary for several metabolic pathways. There is an unconfirmed report of glossitis in possible Pantothemic deficiency.
Biotin
Biotin is a coenzyme in carboxylation reactions. Papillary atrophy of the tongue is the possible feature of the biotin deficiency.
Niacin
Wheat, nuts, meat, and fish are rich in nicotic acid, the active derivative of is nicotinamide.
It is necessary for the production of NAD and NADP for oxidative metabolism.
Niacin is vital in the normal functioning of CNS, in maintaining the integrity of skin and mucous membranes and especially in supplying the needed coenzyme for the energy cycles.
Pellagra is a niacin deficiency disease caused by a primary inadequate dietary intake or by a secondary conditioning factor such as alcoholism, GIT disease, hyperthyroidism, or infection that inhibits absorption and use of nutrition.
Pellagra – 4Ds dermatitis, diarrhoea, depression and death.
Early symptoms include; weakness, persistent fatigability, irritability, headache and depression. Soreness and inflammation of the tongue and mouth aggravated by highly seasoned food is also a frequent complaint. Dermatitis tends to be most severe in areas of exposure to chronic irritation, sun, or heat. The most likely to be affected parts are hands back, face, neck, wrist, elbows, knees. The lesions are usually symmetrical. At first, there is reddening of skin and thickening, followed by variegated dermatitis with brown, scaly areas alternating with areas of depigmented, shiny, shrunken skin.
The tongue is sore, swollen, scarlet in color, and smooth secondary infection with fungi or bacteria characteristic of ANUG is common.
Diarrhea is due to the inflammation of the mucosal lining of the esophagus, stomach, and colon. Depression, confusion, hallucinations, and delirium can result from the degeneration of nerve and brain cells.
Toxicity
Nicotinic acid can cause a transitory dilation of blood vessels, resulting in tingling and flushing of the skin.
Vitamin B12 (Cobalamin)
Function
Vitamin B12 is a coenzyme involved in the synthesis of nucleoproteins by participating in the metabolism of purines and pyrimidines.
Vit. B12 is necessary for the synthesis of thymidine, the nucleotide of thymine, which is the characteristic base of DNA. In general, it affects cells that are dividing rapidly, such as those dealing with the formation of blood, and in its absence, there is a block in DNA synthesis that results in megaloblastic hematopoiesis.
Vit. B12 plays a biochemical role in the maintenance of myelin sheath around nerve fibers.
Deficiency
Occurs in the absence of intrinsic factor which is required for the absorption of Vit. B12.
Shrunken gastric mucosa as in elders, tapeworms
Malabsorption syndromes such as sprue, intestinal inflammation, and strictures.
Pernicious anemia is a disease in with an intrinsic factor is not produced and, consequently, Vit. B12 is not absorbed. Deficiency can be detected by the presence of megaloblasts in bone marrow biopsy specimens. When megaloblasts are present in bone marrow, the RBC in the peripheral circulation is usually macrocytic. There are atrophic changes in the alimentary tract, and in CNS, there is myelin degeneration of the spinal cord.
Clinically, patients with pernicious anemia have
- Difficulty in walking
- Weakness, numbness, and tingling in the extremities.
- Vibratory sense may be absent
- Lemon yellow complexion
- Early graying of hair
- ankle swelling
- Peripheral neuritis
The patient also has a bright red, smooth, sore, and burning tongue resulting from atrophic glossitis. The tongue is called a beefy tongue. Angular stomatitis, aphthae, and erosive lesions may also be seen.
Diagnostic laboratory tests
- Low gastric acidity, even after administration of histamine
- Some megaloblastic RBC
- Oval shaped red cells
- Greatly segmented neutrophils
- Increase MCV
- positive schilling test
- The schilling radioactive B12 absorption and excretion test is conducted as follows.
A measured amount of radioactive Vit. B12 is given orally, followed by a 1mg-dose of the non-radioactive vitamin. The % of radioactivity is determined in the urine excreted over a 24 hour period. Normal people excrete 10-40% of the B12 given, whereas patients are pernicious anemia retain most of the Vit. B12, excreting <1%.
To prove that the absorption failure is due to lack of intrinsic factor, the test is repeated with labeled B12 accompanied by normal gastric juice or a concentrated intrinsic factor which should restore absorption to normal.
RDA
3 ug of B12 /day – adults
4 ug /day – pregnants
Vit. B12 – does not found in plants that occur primarily in animal foods, and the liver is the richest source. Meat, egg, fish milk, cheese good sources of this vitamin.
Vitamin C – (ascorbic acid)
Water-soluble vitamin
Found in fresh vegetables and citrons fruits.
Function
Role in the synthesis of collagen
It also contributes to the integrity of cells associated with fibroblasts, osteoblasts, and odontoblasts; these are the cells that are respectively involved in the development of CT, bone, and teeth.
Collagen synthesis
Collagen is the main organic component of the extracellular matrices of many tissues, including bone, teeth, and the gingival. Vit. C appears to play a role in the synthesis of collagen. Vit. C is necessary for hydroxylation of proline and lysine to form hydroxyproline and hydroxylysine, the essential precursors for the collagen biosynthesis.
Because collagen is the matrix in with calcium is deposited to form bones, a deficiency in Vit. C would impair their formation and could even cause the bone to fracture easily.
Vit. C enhances Iron absorption and plays a number of roles that relate to hematology
Vit C is involved in phagocytosis and acts as a detoxifying agent.
The participation of Vit. C in the synthesis of hormones by the adrenal gland may account for the high concentration of Vit. C in adrenal tissues.
Vit. C plays an important role in the metabolism of tyrosine.
Wound healing
The first step in wound healing is the accumulation of ground substance. In normal animals, this accumulation rises rapidly during the first 3 to 4 days and then begins to decline, with the decline of ground substance formation, fiber formation begins. In contrast to normal wound healing, the animal with a survey experiences a continued increase in ground substance beyond the fourth day. This ground substance surrounds the fibril and prevents fiber synthesis.
Thus, a scorbutic wound differs from a normal wound in that there is a marked decrease if not a total absence of collagen fibrils, and a large amount of amorphous material in the intercellular space.
Oral signs of Vit. C deficiency
Gingival and Periodontal tissues :
The characteristic oral sign of scurvy is an enlargement of the marginal gingivae that envelops and almost completely conceals the teeth. The gingivae are bluish-red, fragile capillaries. Soft and hemorrhage spontaneously and with a slight provocation.
The inflamed gums can become secondarily infected by organisms that will result in acute necrotizing gingivitis clinically, characteristic “punched out,” membranous interdental papillae, and fetid breath.
On x-ray, there is evidence of interruption of lamina dura, suggesting a disturbance of periodontal collagen. Gingivitis with hemorrhagic, enlarged bluish-red bluish-red gingivae is a classic sign of scurvy, but gingivitis is not caused by a lack of Vit. C, per se as such…
Teeth :
The effect of Vit. C deficiency has been demonstrated histologically on the guinea pig incisor tooth, with grows 2mm each week. Odontoblasts atrophy, thereby producing a haphazard irregularity in the usual orderly palisade arrangement, with results in irregular dentin or no dentin at al.
Dietary allowance – RDA for Vit. A is = 60mg/day between 15 to 60 age group 45-50 mg/day up to 21 years.
80 mg/day for pregnant
Food Sources
Green pepper, red pepper, cabbage, spinach, peas, beans, tomatoes, strawberries, carrots, turnips, potatoes.
Role of Proteins in Oral Health
The oral cavity is unique in structure lined by mucous membrane and contains the teeth. The mucous membrane is made up of epithelium and connective tissue.
Masticatory epithelia are often keratinized (Example attached gingiva and hard palate).
In epithelia, which are touching to keratinize, the stratum Spinosum cells fuse into the stratum granulosum in which keratohyalin granules appear in the cytoplasm.
The main difference during keratinization is the conversion of the intracellular protein, keratin from a hydrated structure, harmonious with the life of cells, to a strong extremely insoluble protein which fills the region inside the shrunken epithelial cells of the stratum corneum layer more/less completely, under the control of hydrolytic enzymes. But the mechanism is not known.
Because stratum corneum is the keratin layer, its teeth include fully cornified, shrunken, flattened, and featureless cells.
The main purpose of keratin is to preserve the surface with a layer that is physically strong, coherent, and relatively invulnerable to both microorganisms and substances in solution.
The keratin molecule includes a giant proportion of S-S bridges connecting the different polypeptide chains providing mechanical strength. If these bridges are broken, there is an increase in solubility and a decrease in tensile strength.
Since masticatory mucosa is subjected to bear forces generated when food is chewed, keratinization helps it to withstand these forces i.e. the keratin, a protein. Keratin is made up of Asp., Thr. Ser. Glu, Pro, Gly, Alq, Half, cystine, val, met, Ilev, Leu, Tyr. Pal, His, Lys, Arg, Amide.
Enamel
Proteins play a very important role in the mineralization and maturation of enamel. In the secretory phase of Amelogenesis, the organic matrix consists of enamel proteins and an array of enzymes, including serine proteases, metalloproteinases, and phosphatases.
Of the enamel proteins,
Amelogenins form 90%
Amelin/Ameloblastin 8%
Enamelin 2%
Tilftelin negligible
Amelogenins are a heterogeneous group of low molecular weight hydrophobic proteins rich in proline, histidine, and glutamine. They form the bulk of the tissue.
Amelogenin is carefully processed, apparently by metalloproteases, concomitant with the crystal growth (hydroxyapatite). Their main function is to support and locate the developing framework of the developing crystals.
During maturation, they flow under pressure because of their chemical composition and squeezed out from between the growing crystals.
So also, the proteases secreted by the ameloblasts degrade amelogenins to lower molecular weight proteins like tyrosine rich amelogenin polypeptide (TRAP) and lysine-rich amelogenin polypeptide (LRAP) which can also be more easily removed from between the crystals.
In this way, most of the organic material is removed from the enamel leaving behind TRAP & LRAP residues as a surface coating surrounding the crystallites in a full nature enamel matrix.
Amelin/ameloblastin plays a similar role in prism development
Enamelin/Tuftelin is insufficient to interact with the surface of the crystal present.
The role of enamel proteins is
- To determine the nature and direction of crystal growth within enamel and
- To flow away from the pressure excreted by the enlarging crystals.
This simply implies that deficiency of these proteins will lead to the hypomineralisation of enamel. The consequences of which are.
A soft and friable enamel which can be removed by a prophylaxis instrument.
The enamel not formed to full normal thickness leading to smaller teeth prone to caries.
Dentin
Dentin consists of 65% of inorganic matter, 35% of organic matter, which consists of
A ground substance composed of mucopolysaccharides (proteoglycans and glycosaminoglycans) and
Collagen fibrils
Collagen and ground substance plays an important role in the mineralization of dentin because the earliest deposition of hydroxyapatite crystals takes place on the surface of collagen fibrils and in the ground substance.
Subsequently, crystals are laid down within the fibrils with the long axis of crystals parallel to the long axis of fibrils in an orderly fashion.
Inadequate collagen will lead to imperfect dentin which clinically gives the teeth -brownish violet to a yellowish-brown color
Enamel is chipped off because of inadequate support from the underlying dentin, mainly because of an abnormal DEJ.
Pulp
The pulp consists of cell (fibroblasts, undifferentiated mesenchymal cells) and intercellular substances.
This intercellular substance is dense and gel-like in nature composed of both acid mucopolysaccharides and protein-polysaccharide compounds (glycosaminoglycans and proteoglycans)
The ground substance lends support to the cells of the pulp, so it serves as a means for transport of nutrients from the blood vessels to the cells, as well as for transport of metabolites from cells to blood vessels.
Role of Protein in the Biochemistry of Periodontal tissues
Periodontal tissues consist of two mineralized – cementum and bone and two fibrous elements i,e gingiva and periodontal ligament.
It is composed of epithelium and connective tissue
The epithelium of the gingival sulcus is the junctional epithelium adheres to the tooth surface by Physico-chemical forces mediated by proteins.
Connective tissue consisting of cells and fibers embedded in a ground substance composed of serum proteins, Glycoproteins are associated with oligosaccharides
Myeloproteins contain such acid mucopolysaccharides as hyaluronic acid and chondroitin sulfate.
Mucoproteins are essential for the maintenance of a regular distribution of H2O & electrolyte in the tissues and also to bind collagen fibrils to fibers by cross-linking. Glycoproteins are associated with cell adhesion.
Alveolar bone
It provides rigidity to the periodontium, and collagen is required for bone crystallization because the bone is sensitive to change in protein metabolism.
Saliva
Saliva contains inorganic and organic constituents. The organic constituents of saliva are the proteins which amount to 0.15 – 0.25g/100ml.
Many of them are glycoproteins, which are responsible for the viscosity and lubricating properties of saliva.
Glycoproteins contain 1/more heterosaccharide side chains, covalently bonded to a protein backbone. The side chains may be branched and include a comparatively little amount of sugar excesses. They often end with a sialic acid residue.
The long rod-like structure of glycoprotein molecules and their tendency to aggregate in solution are responsible for the characteristic physical properties of saliva.
Oral lesions in Protein-energy malnutrition
- The pallor of the lips, tongue and oral mucosa
- Atrophy of lingual papilla.
- Variable degree of hyperkeratosis of the oral mucosa
- Enamel dysplasia, especially hypoplastic defects of the primary dentition
- Fissuring of the lips
- Angular cheilosis
- Glossitis
- Generalized stomatitis may also be seen.
- Gingivitis and periodontitis are more severe than those seen, because of the presence of local factors associated with plaque.
- Radiographically, marked resorption of the interdental septa can be noticed.
Other oral lesions associated with PEM are
- Necrotizing Gingivitis
- Cancrum oris
- Abnormal dental growth and development
ANUG
It is a socio-economic lesion affecting the underprivileged children who generally have poor oral hygiene status and are chronically malnourished. The disease is characterized by the development of painful, hyperemic gingival and sharply punched-out erosions of the interdental papillae, covered by gray, necrotic pseudomembrane and bleeds when touched.
Cancrum Oris/Noma
It is a rapidly spreading gangrene of the oral and facial tissues that occurs usually in nutritionally deficient persons chiefly children. It is an infection by vincents organisms with a secondary invasion of other microbial forms, including streptococci, staphylococci, and diptheria bacilli.
Noma begins as a small ulcer of the gingival mucosa with rapidly spreads and involves surrounding tissues of the jaws, lips, and cheeks by gangrenous necrosis.
Abnormal Dental Growth And Development
71% of infants whose mothers had a poor protein diet during pregnancy had retarded the development of bone and teeth. If the diet includes too little/none of the essential amino acids during the critical period of active growth, permanent structural damage can occur. Synthesis of protein in the cell is disrupted, resulting in disturbed tissue growth and development.
For example, when an infant is usually going from low protein liquid food and (milk with 5% protein) to a high protein solid food and (meat with 20% protein), if solid protein-rich food eating is not fair, jaw and tooth deformities are likely.
Lack of growth – from chewing firm foods may also be a factor. Teeth tend to be crowded and rotated, possibly caused by inadequate development of jaw bone. Newly forming bone tissue is extremely sensitive to protein deprivation. Teeth of normal size in an undersized jaw will produce a crowded arch. Delayed eruption and hypoplasia of deciduous teeth are also noted. Teeth are smaller and more caries prone.
In experiments on feeding protein-deficient diets to rats, stringent deficiencies of amino acids lysine and tryptophan produced an irregular predentin layer and a number of interglobular spaces in a poorly calcified dentinal matrix.
Effect of protein deficiency on Dental caries
In experimental animals, a protein-deficient diet increases caries susceptibility either by a quality defect in the matrix of the tooth enamel or by alterations in the salivary gland.
In humans, there is no direct evidence of a correlation between dental caries experience and dietary supplements of protein.
Effect of Protein on Periodontal diseases
Finding the correlation between periodontal health in humans and their protein status is inconclusive and controversial because of the number of uncontrollable variables involved in the causes of periodontal disease
As Stahl states, “Nutritional deficiencies apparently do not initiate periodontal disease, but may modify the severity and extent of the lesion by altering the resistance and repair potential of the affected local tissues.
CARBOHYDRATES
Polysaccharides
By functioning as a structural agent in plants, the cellulose that is most commonly occurring CHO in nature provides non-digestible roughage or bulk in the human diet.
The starches (amylase, amylopectin, and glycogen) are digestible by humans, and they provide sources of glucose. More complex CHO, such as Muco polysaccharides and glycoproteins, are associated with the structure in animal tissues.
Disaccharides
Sucrose is the most common of the disaccharides, usually found in sugar cane and beets. It has many functions in food preparations. Eg. : Color, flavor, texture, and preservation. Sucrose is hydrolyzed to glucose.
Lactose is disaccharide found in milk. It is a dietary source of galactose and glucose. Maltose is a disaccharide that is found in malt and germinating cereals. It can be hydrolyzed to glucose.
Monosaccharides
Hexoses
The major function of the three common monosaccharides (glucose, fructose, galactose) is to provide glucose as a source of energy. The majority of both fructose and galactose molecules ultimately end up as glucose. Some galactose is used in the synthesis of glycolipids, glycoproteins, and lactose in the mammary glands.
Of the monosaccharides, glucose is one of the greatest metabolic importance in humans. It is the efficiently utilized source of acetate for Kreb’s cycle.
Glucuronic acid derived from glucose of the liver is used by the body to detoxify certain compounds in the liver and to remove them from the body by kidneys. Glucose also serves as a precursor for other metabolites used in the synthesis of such substances, glycerol, and glycogen.
The availability of glucose for energy acts as a regulator for fat and protein metabolism, preventing the build-up of ketones from beta-oxidation and sparing proteins from being used for energy purposes.
Pentoses
The five-carbon sugars (pentoses) are not used in energy metabolism as sources of calories. Instead, they are used in the synthesis of nucleic acids, nucleotides, and nucleoproteins.
Disturbances in CHO metabolism
Almost nothing is known of the effects of CHO deficient diets on the oral structure. Since they form a large part of our diet, they can be considered.
Hurler’s syndrome (Mucopolysaccharidosis I Gargolysm)
It is a disturbance of mucopolysaccharide metabolism exhibiting a variety of classic clinical features.
Clinical features
- Seen in the first two years of life, progresses during childhood and adolescence and terminates in death usually before puberty.
- Head appears large, and facial characteristic is typical.
- – prominent forehead, Broad saddle nose, wide nostrils
- Hypertelorism
- Puffy eyelids with rough bushy eyebrows, thick lips, large tongue, open mouth, nasal congestion with noisy breathing
- Progressive corneal crowding
- Hepatosplenomegaly – protuberant abdomen.
- Short neck, Claw hand, Mental retardation
Oral Manifestations
Shortening and broadening of the mandible with prominent gonions, the broad intergonial distance around the arch – regular spacing of teeth. Some regions of bone destruction in the jaws may be seen, which seem to express hyperplastic dental follicles with huge puddles of metachromatic matter, apparently mucopolysaccharides.
The teeth are a small – delayed eruption, gingival hyperplasia.
Lipid proteinosis (Hyalinoss cutis et mucosae)
Lipid proteinosis is a disease thought to represent a disturbance in mucopolysaccharide metabolism.
Clinical features
Yellowish white waxy material varying in size from minute to 0.5cm on the skin of the face, neck, hands, axilla, scrotum, perineal areas, and intergluteal clefts.
Oral Manifestations
Oral Mucous membrane developing the characteristic yellowish, white, papular plaques, which become increasingly more prevalent. The lips become thickened and nodular. The tongue becomes thickened, enlarged.
Recurrent painful parotitis.
Congenital absence of teeth and severe enamel hypoplasia
Hereditary Fructose Intolerance
Clinical features
Autosomal recessive trait and is manifested by hypoglycemia and vomiting after fructose-containing foods.
Oral Manifestations
Increase caries activity.
LIPIDS
Simple lipids
Fattyacids: The basic subunits of lipids are fatty acids. At 9 calories per gram, fats store more than twice the calories of carbohydrates.
Fatty acids range in length from 4 carbon to 24 carbon. Energy storage is its main function. Certain fatty acids (Linoleic acid, linolenic, and arachidonic acid) have been considered essential. These F.A are used to synthesize all membranes and more complex lipid metabolites such as prostaglandins. Fatty acid levels in the blood have been associated with appetite control.
Neutral Fats
Fatty acids and glycerol combine to form triacylglycerols (Triglycerides), diglycerol (diglycerides), and monoacyl glycerols (monoglycerides). The acylglycerols are basically transport and storage forms of fat. They play an important role in solubility during the absorption and transportation of fat-soluble vitamins. Adipose tissue is the site of storage for these lipids such tissues serves as thermal insulation. Additionally, adipose tissue protects and supports internal organs. Although glucose is used first as the preferred energy source, most of the body’s energy stores are in adipose tissue as neutral fat.
Compound lipids
Phospho lipids: The most important functions of phospholipids are in membrane structure and transport.
Glycolipids: They contain carbohydrates, generally glucose or galactose. They also function in membrane structure and transport.
Lipoproteins :
These are primarily involved with lipid and cholesterol transport throughout the body.
Derived lipids
This is a complex group of lipid compounds that includes cholesterol, steroids, hormones, bile salts, and fat-soluble vitamins.
Cholesterol is a precursor or intermediate to the production of steroid hormone, Vit. D and bile salts.
Disturbances in lipid metabolism
Lipid metabolism is concerned with the assimilation, utilization, replacement, and synthesis of various forms of fatty acids.
Non-lipid reticuloendotheliosis (Histiocytosis X)
Langerhans cell disease, also formerly known as histiocytosis X and idiopathic histiocytosis, is a disorder characterized by a proliferation of cells exhibiting phenotypic characteristics of Langerhans cells.
The clinical manifestations of this process range from solitary or multiple bone lesions to disseminated viscerals, Skin and bone lesions.
Historically, the term histiocytosis X was used to encompass three disorders:
Eosinophilic granuloma
Hand Schuler’s – Christian disease
Letterer – siwe disease
Eosinophilic granuloma has referred to solitary or multiple bone lesions only.
Hand – Schuller Christian syndrome has represented a specific clinical triad of lytic bone lesions, exophthalmos, diabetes insipidus.
Many of the affected persons also exhibited lymphadenopathy, dermatitis, splenomegaly but now,
Letterer – siwe disease, more recently referred to as the acute disseminated form of idiopathic histiocytosis, most likely represents a malignant neoplastic process.
A minority of patients actually present with the classic triad of Hand Schuller Christian syndrome. This chronic disseminated form of the disorders is one of the various presentations in with lymph node, visceral, and bone involvement may occur. Less severe chronic localized forms of idiopathic histiocytosis appear to be represented by cases in with only multifocal or unifocal bone lesions are noted.
Categorization of Langerhans cell disease has also been termed either restricted or extensive based on the clinical extent and site of disease involvement.
Clinical features
- Condition of children and young adults that exhibits extreme clinical heterogeneity.
- Male predominance
- It can affect any bone of the body.
- The skull, mandible ribs, vertebrae, and long bones are frequently involved.
- Oral changes may be the initial presentation in all forms of these disorders.
- Skin, mucosal, or bone involvement in the head and neck region was noted in more than 80% of children in one study.
- Tenderness, pain, and swelling are frequent patient complaints
- Loosening of teeth, Halitosis, unpleasant taste.
- The gingival tissues are frequently inflamed, hyperplastic, and ulcerated.
- Oral mucosal lesions in the form of submucosal nodules, ulcers, and leukoplakia have also been described.
- The jaws may exhibit solitary or multiple radiolucent lesions. The lesions frequently affect the alveolar bone, causing the teeth to appear as if they floating in space.
- Bone lesions with a sharply circumscribed punched out appearance may also occur in central aspects of maxilla and mandible. These lesions are usually located in periapical areas.
- Jaw lesions may be accompanied by bone involvement elsewhere in the skeleton.
- Cervical lymphadenopathy, mastoiditis, and otitis media are head and neck manifestations frequently present with multifocal involvement.
- Failure of healing of extraction sockets
Etiology
Remains obscure
Some cases represent a neoplastic transformation
Role of virus i.e. herpes virus 6.
Cell-mediated immune defects
Thymic abnormalities
Histopathology
The proliferation of large cell with abundant cytoplasm, indistinct cell borders
The second population of mononuclear phagocytes is frequently evident
Multinucleated giant cells and foci of necrosis present
Electron microscopy shows the presence of rod-shaped cytoplasmic structures called Birbeck granules inside Langerhans cells.
Gaucher’s disease
An autosomal recessive disease of lipid metabolism
Niemann pick disease
Least common of genetic disturbances of lipid metabolism. It is an autosomal recessive trait.
TRACE ELEMENTS
Trace minerals or elements, or micro minerals, are inorganic nutrients that are required by humans in very small amounts (from micrograms to no more than a few milligrams).
A trace mineral is essential for humans when it has a vital function and is required to avoid a deficiency disease.
Mode of action
Trace elements act as catalysts, either as metalloenzymes or as metal enzymes.
Example: Iron, Zinc, Copper, and Molybdenum – Metaloenzyme (in which trace element is an integral part of the enzyme molecule).
Metal – the enzyme is – Arginase (in with the metal ion is loosely associated with the enzyme)
Trace elements also function as constituents and activators of hormones.
Selenium
It has an antioxidant property. It is an essential compound of the enzyme that catalyzes the oxidation of glutathione. Glutathione protects RBC through the destruction of H2O2, thus protecting Hb from oxidation damage.
Molybdenum
Molybdenum is part of the molecular structure of 2 enzymes, xanthine oxidase, and aldolase oxidase. Xanthine oxidase is responsible for the conversion of xanthine to uric acid. It is an essential nutrient for humans.
Chromium
Chromium is required for the maintenance of normal glucose and energy metabolism in experimental animals. It may acts as a cofactor in insulin.
Copper
Normal amount is 100 to 150 mg in body functions:
Aid in the synthesis of Hb in bone narrow
Form and maintain compounds having enzymatic activity
Influence CNS physiology
Aid in the formation of pigments
Excess Is called Wilson’s disease – accumulation of excess copper in the body tissue, probably because of the genetic absence of a liver enzyme.
Clinical features
Neurological degeneration
Cirrhotic liver changes
Oral effects of imbalance
Concentration in excess of the normal amounts found in human saliva appears to inhibit acid production. Frank copper Deficiency has never been demonstrated in adults
Cobalt
Cobalt is considered an essential trace element because it is part of the Vitamin B12 molecule.
Manganese
It is needed for normal bone structure, for reproduction and for normal functioning of CNS. Mg deficiency produces skeletal abnormalities in animals. The basic defect is in cartilage or bone matrix formation.
Iodine
The adult body contains 15-30mg of iodine. Iodine is a fundamental element of the thyroid hormones. In the absence of iodine, the thyroid gland increases secretory activity to compensate, and enlargement occurs called as hypothyroidism or hyperthyroidism.
Oral effects of imbalance
In severe hypothyroidism – jaws are small and delayed tooth eruption.
Trace elements that may inhibit or promote Dental caries
Caries supporting elements – selenium, magnesium, cadmium, platinum, lead, silicon.
Element that is mildly cariostatic -molybdenum, vanadium, strontium, calcium, boron, lithium, gold.
Elements with a suspicious consequence on caries -beryllium, cobalt, manganese, tin, Zinc, bromine, iodine.
Caries inert elements – barium, aluminum, nickel, iron.
Elements that are strongly cariostatic – fluorine, phosphors
IRON
Dietary iron is found mainly in meat. Iron is vital to oxygen (O2) transport, intracellular respiration and is inherent in some enzymes such as cytochrome a,b,c, cytochrome oxidase, catalase, peroxidase, and some flavoproteins.
Most iron is present in Hb, and some are stored in macrophages in the liver and spleen as ferritin and hemosiderin.
Deficiency is common and can arise from dietary or as a consequence of chronic blood loss. Iron deficiency affects rapidly dividing cells, such as bone marrow and oral mucosa.
Oral mucosal manifestation include
Glossitis
Angular stomatitis
Aphthae
Burning mouth syndrome
ZINC
Zn is involved in several enzymatic reactions. Deficiency is uncommon and usually dietary or due to inherited disorders like acrodermatitis enteropathica. Zn deficiency can produce ulcerations and impaired taste function and slow healing of wounds.
CALCIUM
Calcium plays a large role in the formation of bones and teeth, in the maintenance of a normal skeletal structure, tooth structure, normal membrane permeability, normal heart rhythm, and others neuromuscular excitability and in coagulation of blood. Variations of serum calcium ion concentration from the limited optimal range of 9 to 11 mg/dl have profound effects.
A low level of calcium levels about 8mg/dl produces hyper-irritability and tetany with characteristic carpopedal spasm and at times, laryngospasm and convulsions, while a high concentration produces depressed nerve conductivity and muscle rigor. The level of blood calcium is largely controlled by the action of parathyroid glands, which are stimulated by low serum calcium levels and inhibited by high serum calcium levels.
Requirements :
360 mg – Newborn
800 mg – children, adults
1200 mg – pregnant, lactating mothers
Disorders of calcium metabolism
Hyperparathyroidism,
In this, there is hypocalcemia as well as reciprocal hypophosphatemia. In urine, there is hypercalciuria and hyperphosphaturia. Serum alkaline phosphate levels may be elevated.
In hypoparathyroidism,
There is pronounced hypocalcemia, and tetany may follow.
In rickets, in children, serum calcium may be normal or lowered, but serum phosphorus is definitely lowered. But in osteomalacia, serum calcium is lowered, and tetany may occur.
Renal rickets is a familial condition and a sex-linked dominant trait; the features are hypophosphatemia, hyperphosphaturia, and reduced intestinal absorption of Calcium and phosphorous.
Osteoporosis and calcium deficiency
The etiology of osteoporosis was thought to be a lack of adequate bone matrix. Recent evidence indicates, however, that it may be due to long term negative calcium balance.
Skeletal mass at old age is proportional to skeletal mass at maturity, indicating that infant and childhood calcium intake may play a major role in the occurrence and severity of the disease in later years.
Phosphorous
Although most of the body phosphorous is intimately associated with calcium in the metabolism of bones and teeth, a much higher proportion of phosphorus is concerned with other vital processes. Phosphates make an in-between step in the metabolism of fats and carbohydrates by their role in phosphorylation.
Phosphates are utilized in the formation of phosphoproteins, such as milk casein, and in the formation of the nerve phosphatides and nucleoproteins of the cells. They provide the energy-rich bonds in such compounds as adenosine triphosphate, which is important in muscle contraction, and they form a part of pyridoxal phosphate, which is necessary for decarboxylation and transamination of certain amino acids such as tyrosine, tryptophan, etc.
Levels: Adults – 2 to 4 mg/dl
Child – 3 – 5 mg/dl.
Requirements: daily intake
240mg – infants
800 mg – adults
Phosphate depletion in man is non-existent under most dietary regimens. Long term antacids will, however, render phosphate unabsorbable.
Effects of diet and Nutrition on oral cancer – Nutrition and oral health
The genetic mutations, under expressions and over expressions underlying carcinogenesis, are precipitated by inherited predisposition and a variety of environmental agents, notably tobacco and alcohol, but also nutritional /dietary and other factors.
Example: A diet low in total fat and high in complex CHO and fiber may reduce the excretion of bile salts into the gut, which may reduce the risk of cancer of the colon.
Foods and additives may contain carcinogens, cocarcinogens, and promoters.
Uncooked foods contain carcinogens derived from fungal contamination, fertilizers, and pesticides, for example, Aflatoxin, B, formed in peanuts and other food contaminated by aspergillus flavus, is a highly potent carcinogen. Hydrazines found in some mushrooms produce carcinogenic and mutagenic derivatives
Preservatives, including nitrates and nitrites, may result in the formation of nitrosamines. Nitrites are present in cured meats and baked foods. Nitro amines are potent carcinogens.
The process of cooking, including frying and roasting, may result in measurable levels of potentially carcinogenic by-products of the pyrolysis of fat and amino acids.
Anemia may influence cancer incidence via several pathways. The Plummer Vinson (Patterson-kelly) syndrome leads to mucosal changes and increased pharyngeal cancer. Malnutrition or anemia may reduce the ability of the immune system to counteract neoplastic cells.
Nutrition and the teeth – Nutrition and oral health
A cross-sectional study of children in Lima, Pero, found that malnourishment delayed tooth development, eruption, and increased caries experience in primary teeth.
Nutrition and orofacial skeleton
A variety of nutrient deprivations or excesses and systemic disturbances can produce congenital anomaly in animals. Underfed children have shorter extremities in relation to total height, and cranial growth is retarded, resulting in smaller head circumference. Low-calorie diets retard the development and eruption of teeth in rats. Mediolateral maxillary growth seems dependent on the vascular stimulation provided by rough elements in the diet. The functional stimulus during vigorous chewing is essential for the growth, development, and maintenance of the orofacial skeleton.
Effects of diet and nutrition on periodontal health – Nutrition and oral health
Diet and nutrition can affect periodontium by influencing plaque bacteria, immunological response, and healing and repair. The eating firm, fibrous foods may be beneficial to periodontal health, whereas soft, sticky foods may be detrimental.
Oral retention of food may be lessened by chewing fibrous foods, due to the friction of chewing and increased salivary flow and amylase activity, but plaque retention is unaffected.
Diet can affect the composition of supragingival plaque through the subgingival plaque is affected only indirectly.
Subclinical deficiencies of folic acid, Vit. C or iron may impair polymorphonuclear leukocyte function.
A Link of zinc deficiency with an increased prevalence of pdl disease might possibly be associated with the role of Zn in regulating the inflammatory process by inhibiting lysosomal release from polymorphonuclear leukocytes.
Oral disease can interfere with feeding and nutrition; conversely, nutritional deficiencies can impair oral mucosal health and oral immune defenses.
ปั้มไลค์
28 Jun 2020Like!! Really appreciate you sharing this blog post.Really thank you! Keep writing.