RESIDUAL RIDGE RESORPTION
We don’t come across the ideal ridge in complete denture patients. 7 out of 10 completely edentulous patients have resorbed mandibular ridge. So you need to understand the residual ridge resorption.
Residual ridge resorption is a normal physiologic process and is not a disease. But this is labeled as a disease because of the wide variation in the rate of residual ridge resorption.
Definition
According to GPT-7, “residual ridge resorption is a term used for the diminishing quantity and quality of the residual ridge after the teeth are removed.”
Classification
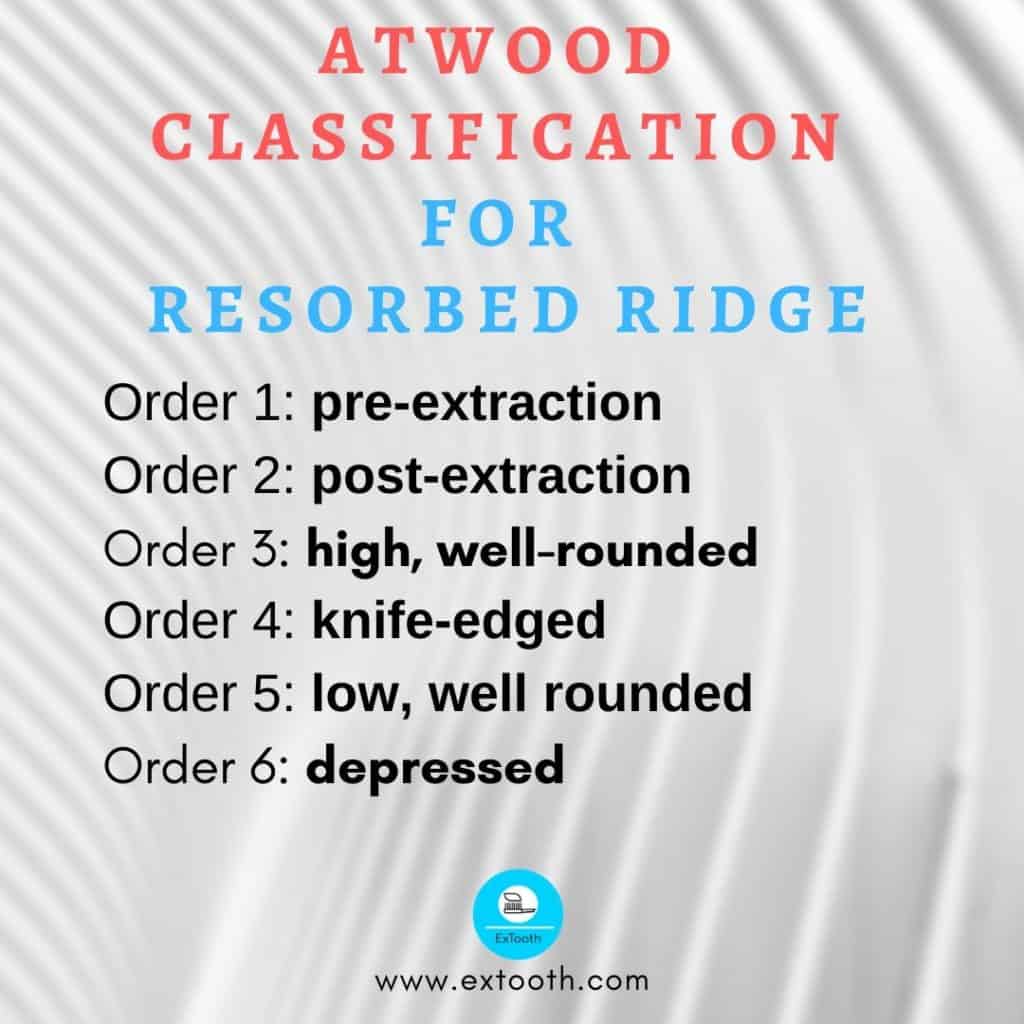
Atwood classified residual ridge resorption into:
Order 1: pre-extraction
Order 2: post-extraction
Order 3: high, well-rounded
Order 4: knife-edged
Order 5: low, well rounded
Order 6: depressed
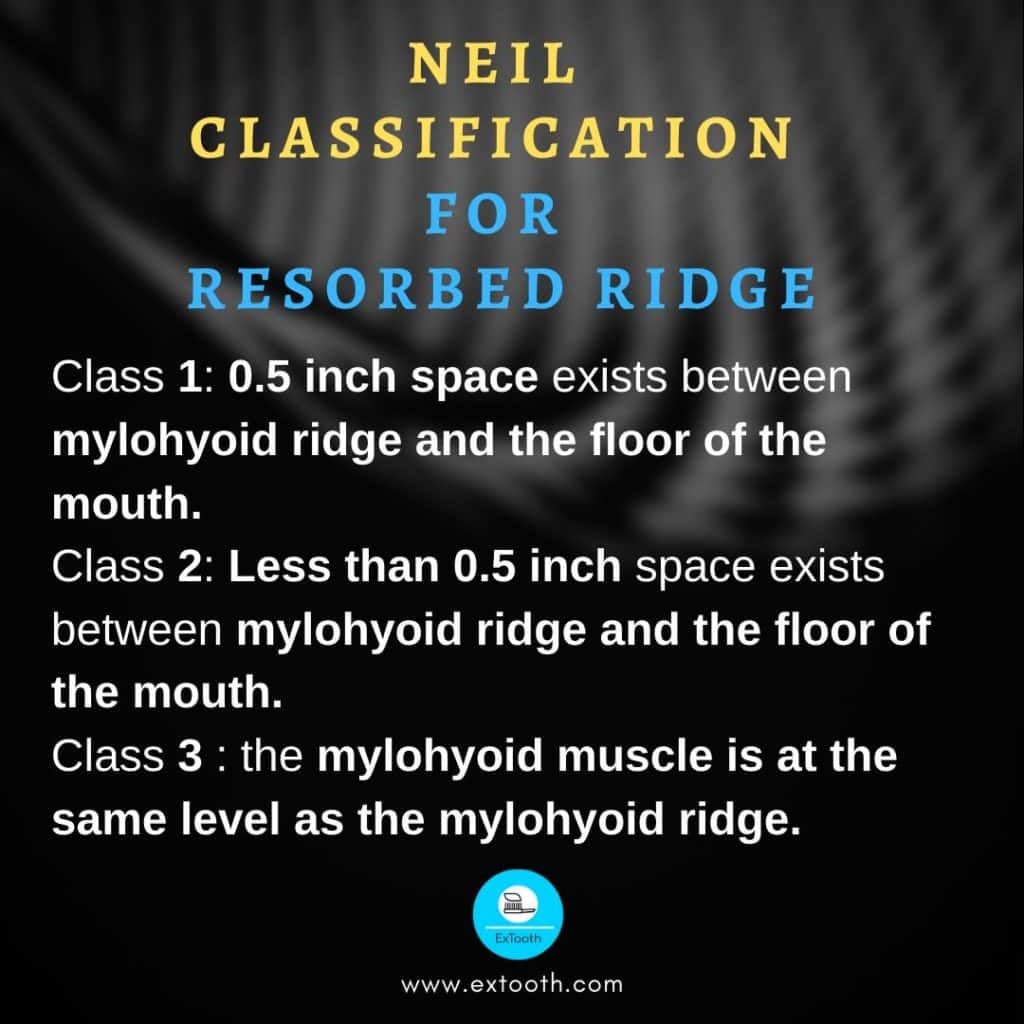
Neil classified residual ridge resorption in relation with the floor of the mouth and mylohyoid ridge:
Class 1: 0.5 inch space exists between mylohyoid ridge and the floor of the mouth.
Class 2: Less than 0.5 inch space exists between mylohyoid ridge and the floor of the mouth.
Class 3: the mylohyoid muscle is at the same level as the mylohyoid ridge.
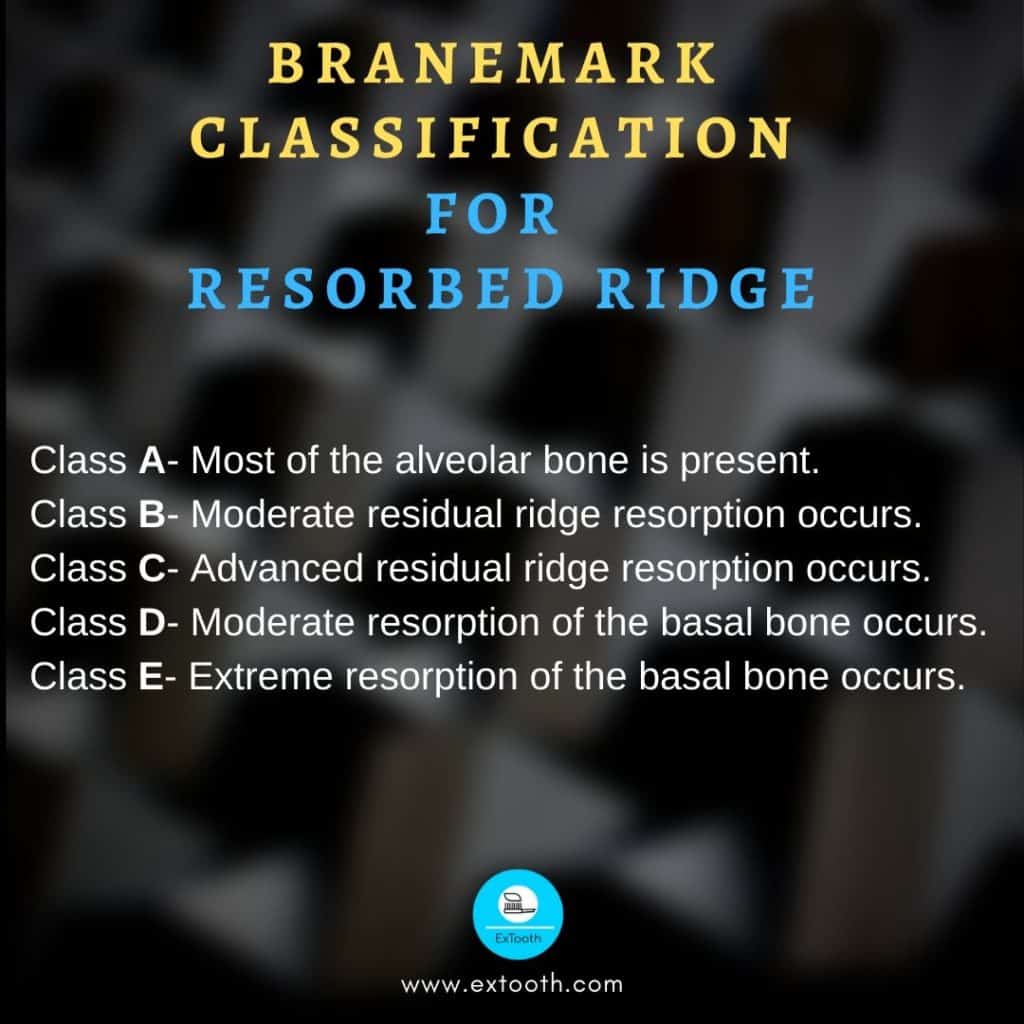
Branemark classified residual ridge resorption depending on bone quality and quantity:
Bone quantity
Class A- Most utmost of the alveolar bone is present.
Class B- Moderate residual ridge resorption occurs.
Class C- Advanced residual ridge resorption occurs.
Class D- Moderate resorption of the basal bone occurs.
Class E- Extreme resorption of the basal bone occurs.
Bone quality
Class 1- Nearly the whole jaw is formed of homogenous compact bone.
Class 2- a thick layer of compact bone encompasses a core of dense trabecular bone.
Class 3- a thin layer of compact bone surrounds a core of dense trabecular bone.
Class 4- a thin layer of compact bone surrounds a core of low-density trabecular bone.
Pathogenesis
There is a reduction in the size of the residual ridge. Residual ridge resorption is a localized loss of bone structure. To categorize the most common residual ridge configurations, Atwood has described the six orders of residual ridge resorption. But there may be porosities and imperfections in the crestal areas of residual ridges of both maxilla and mandible, no matter at what stage of configuration they are. Residual ridge resorption does not stop with residual ridge. This ridge resorption can continue till only a thin cortical plate is left on the inferior border of the mandible, and in maxilla it continues till there is no alveolar process left.
Lateral cephalometric radiographs provide an accurate method for determining RRR.
The panoramic radiograph technique described by Wical and Swoope is a simple, useful method for determining RRR.
Procedure
Original alveolar crest height is determined by measuring the distance from the inferior border of mandible to the lower edge of the mental foramen after superimposing both the lateral cephalometric radiographs.
Clinically, the soft tissues overlying the residual ridges may range from normal to inflamed, edematous, ulcerated, indented or abused tissue.
Microscopic studies show the presence of osteoclasts on the external surface of the crest of residual ridges.
Pathophysiology
Bone undergoes constant remodeling throughout life. Normally bone formation is equal to bone resorption. But in osteoporosis bone resorption is greater than bone formation. Residual ridge resorption is a confined pathologic loss of bone that is not built back by removing the causative factors.
Bone remodeling takes place even in the presence of this pathologic osteoclastic activity. A cortical layer of bone is present over the crest of the ridge even during residual ridge resorption, which clearly shows the formation of new bone.
If endosteal bone growth fails to keep pace with external osteoclastic activity, then medullary bone would be exposed resulting in defects on the crest of the ridge.
Pathogenesis
Residual ridge resorption is chronic, progressive, irreversible and cumulative. It proceeds slowly over a long period of time, flowing from one order to the next order.
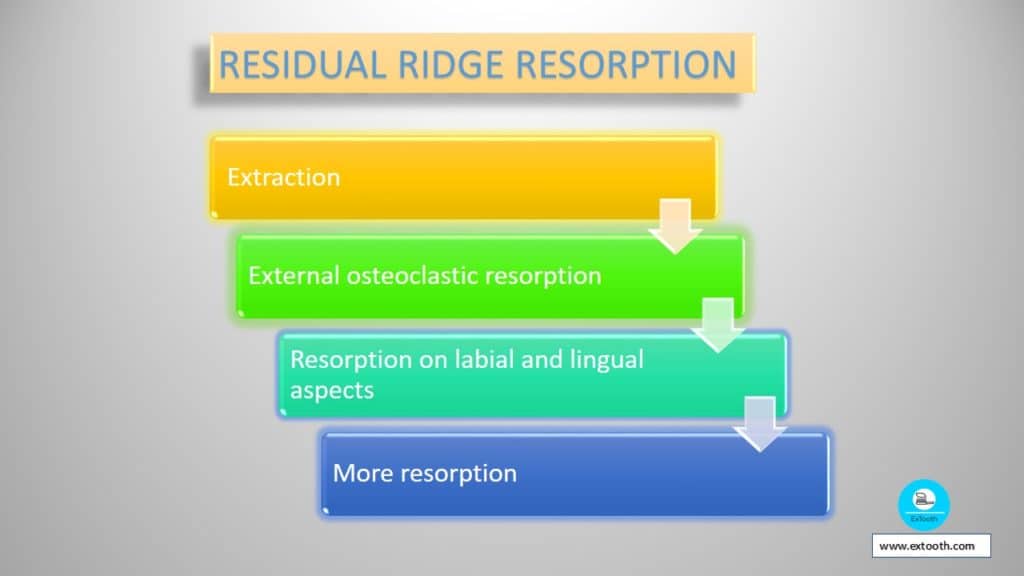
Order 1——order 2——order 3——-order 4——-order 5——order 6
Order 1 to order 2: after extraction
Order 2 to order 3: external osteoclastic resorption
Order 3 to order 4: resorption on labial and lingual aspects
Order 4 to order 5: more resorption
Order 5 to order 6: final stage
Consequences of Residual ridge resorption
Loss of sulcus width and depth with a displacement of the muscle attachment closer to the crest of the residual ridge.
Loss of vertical dimension of occlusion.
Reduction of the lower facial height.
Anterior rotation of the mandible and increase in relative prognathia.
Changes in interalveolar ridge relationship.
Etiology of Residual ridge resorption
Residual ridge resorption is multi factorial and biomechanical disease.
Three major factors lead to residual ridge resorption. They are:
- Anatomic factors
- Metabolic factors
- Mechanical factors
Anatomic factors
Residual ridge resorption and anatomic factors
The presence of more bone will lead to more residual ridge resorption. Large well-rounded ridges and broad palates are favorable anatomic factors for residual ridge resorption.
Metabolic factors
Residual ridge resorption is directly proportional to bone resorption factors/bone formation factors.
Local bone-resorbing factors like endotoxins, osteoclast activating factor (OAF), prostaglandins, human gingival bone- resorption stimulating factor, heparin and trauma lead to residual ridge resorption.
Bone forming factors are circulating estrogen, thyroxine, growth hormone, androgens, calcium, phosphorus, vitamin D, protein and fluoride.
Mechanical factors
Force is the main factor in Residual ridge resorption.
Residual ridge resorption is directly proportional to force
While considering force, one must also consider:
- Amount of force
- Frequency of force
- Duration of force
- Direction of force
- Force per unit area
Also, force applied to the bone is affected inversely by the damping effect of the underlying tissue. The damping effect is energy absorption in the mucoperiosteum.
Residual ridge resorption inversely proportional to damping effect
So residual ridge resorption is related to the etiologic factors in the following manner:
Anatomic factors
+
Residual ridge resorption is directly proportional to Bone resorption factors/bone formation factors
+
Force factors / damping effect factors
+
1 / time
This time is the time taken since extraction to the bone loss in residual ridge resorption.
Treatment
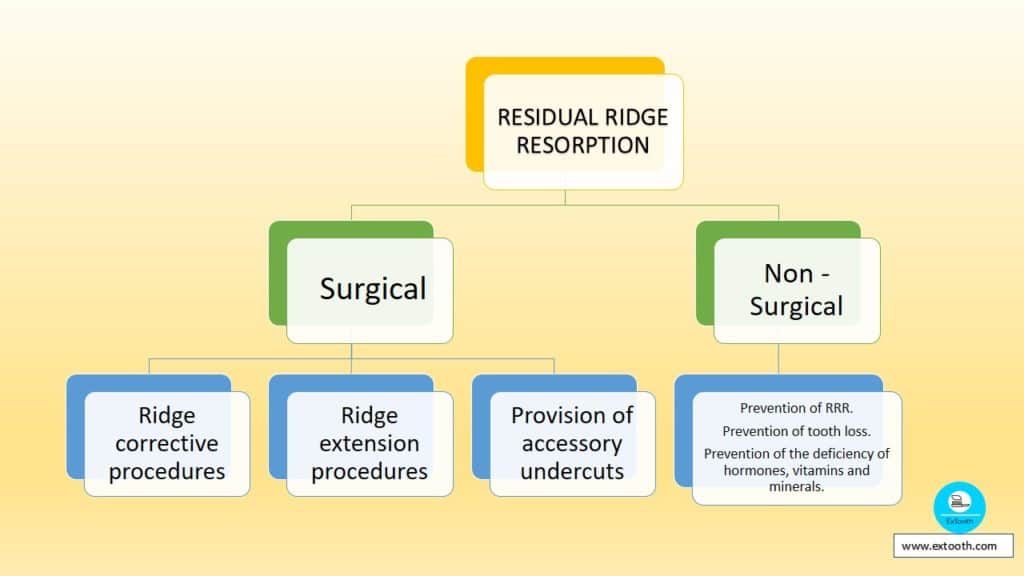
Treatment for residual ridge resorption is of two types:
- Non-surgical
- Surgical
Non-surgical treatment
- Prevention of Residual ridge resorption.
- Prevention of tooth loss.
- Prevention of the deficiency of hormones, vitamins, and minerals.
Surgical treatment
- Ridge corrective procedures
- Ridge extension procedures.
- Provision of accessory undercuts.
Ridge corrective procedures
- Soft tissue correction
- Hard tissue correction
Soft tissue correction
- Labial frenectomy
- Lingual frenectomy
- Mobile tissue on the alveolar ridge
- Enlarged tuberosity
- Enlarged retromolar pad
Hard tissue correction
- Shaping unsuitable bony ridge
- Alveolectomy
- Elimination of unfavorable undercut
- Excision of tori
- Ridge extension procedures
- Vestibuloplasty
- Ridge augmentation procedure
Provision of accessory undercuts
- Creating favorable undercuts
- Dental implants
- Onlay denture
Management of Residual ridge resorption
Ideally, we should treat Residual ridge resorption by preventing it. The best of all is to prevent the loss of natural teeth. But this is highly impossible.
The etiology of Residual ridge resorption being related to the deficiency of some hormone, vitamin or mineral is yet to be discovered & causally related to Residual ridge resorption.
Until this is determined, it is essential to analyze our patients in regard to the various possible factors to best of our ability, to seek consultation concerning possible metabolic factors, & to perform prosthodontic care of our patients within our best capabilities.
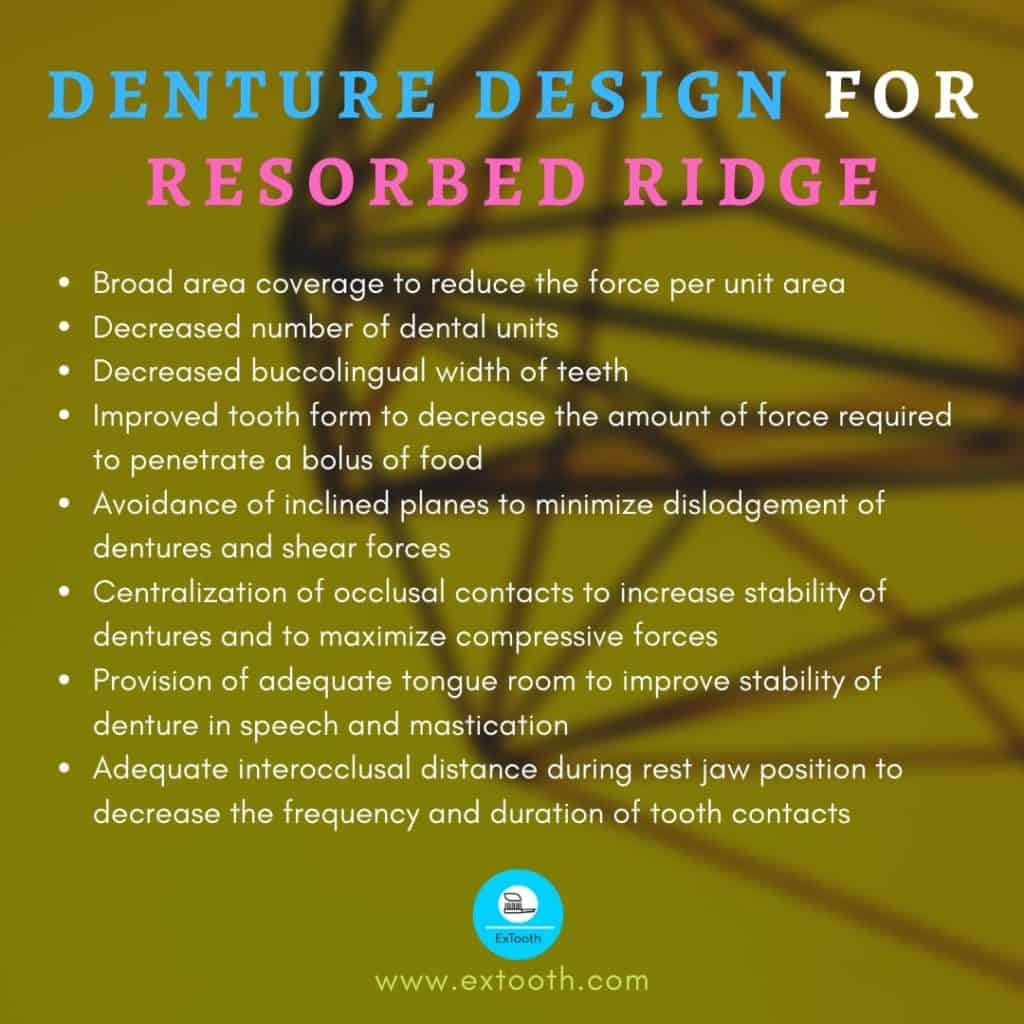
The traditional design of dentures includes many features whose goal is to reduce the amount of force to the ridge & thereby to reduce Residual ridge resorption.
These prosthetic factors include broad coverage area, decreased number of dental units, decreased buccolingual width of the teeth, improved tooth form, avoidance of inclined planes, centralization of occlusal contacts, adequate interocclusal distance during rest jaw relation.
The treatment of a patient with prosthodontic needs can be modified according to the type of ridge present as a result of ridge resorption.
FLAT PALATE WITH SHALLOW RIDGES
the denture may easily be displaced during mastication through lack of ridge support, the shallow sulci adversely influence peripheral seal
Treatment: an impression technique incorporating careful peripheral adaptation, the use of cuspless teeth, to reduce the lateral drag from cuspal interference.
UNDERCUT RIDGES
Retention will be reduced as denture will have to be trimmed, during fitting, in order that it may pass over the bulbous area of the ridge, thus causing loss of peripheral seal.
Treatment: 1. an alveolectomy to reduce undercut.
2. careful blocking out of the undercut areas on the model
KNIFE LIKE LOWER RIDGE
The patients with a ridge of this type frequently complain of pain during mastication as the pressure exerted on the mandible via denture compresses the soft tissue between the fitting surface & the knife-like process forming the crest of the alveolar ridge.
Treatment: 1. alveolectomy to reduce the sharp process
2. relief for the knife-like ridge area
3. construction of denture having resilient lining.
4. reducing the vertical dimension in such cases may be advantageous as this reduces the force applied during mastication.
FLAT LOWER RIDGE
The shape of the ridge provides no resistance to lateral movements of the denture.
Treatment: a peripherally adapted impression having an adequate extension on to the retromolar pads & teeth set up to produce balanced articulation. Non-anatomic teeth should be used for the setup.
OVERDENTURES
Any removable dental prosthesis that covers & rests on one or more remaining natural teeth, the roots of natural teeth, &/or implants.
The overdentures accomplishes three rather obvious, but tremendously important goals
1. It maintains teeth as part of the residual ridge. This gives the patient a denture that has far more support than any conventional appliance. The denture sits on teeth “pilings”, enabling the denture to withstand a much greater occlusal load without movement.
2. A decrease in the rate of resorption. Alveolar bone exists as support of the teeth. If the teeth are removed, then the alveolar process begins the rate of resorption consistent with the time of edentulism. Thus the use of overdentures preserves the alveolar bone.
3. with the preservation of teeth for an overdenture, there is also the preservation of the periodontal membrane that surrounds these teeth. This preserves proprioceptive impulses supplied by the periodontal membrane.
Of all these goals, preservation of the residual ridges is most important.
SURGICAL MANAGEMENT OF RESIDUAL RIDGE RESORPTION
MANDIBULAR AUGMENTATION
- SUPERIOR BORDER AUGMENTATION.
- INFERIOR BORDER AUGMENTATION.
- HYDROXYAPATITE AUGMENTATION.
MAXILLARY AUGMENTATION
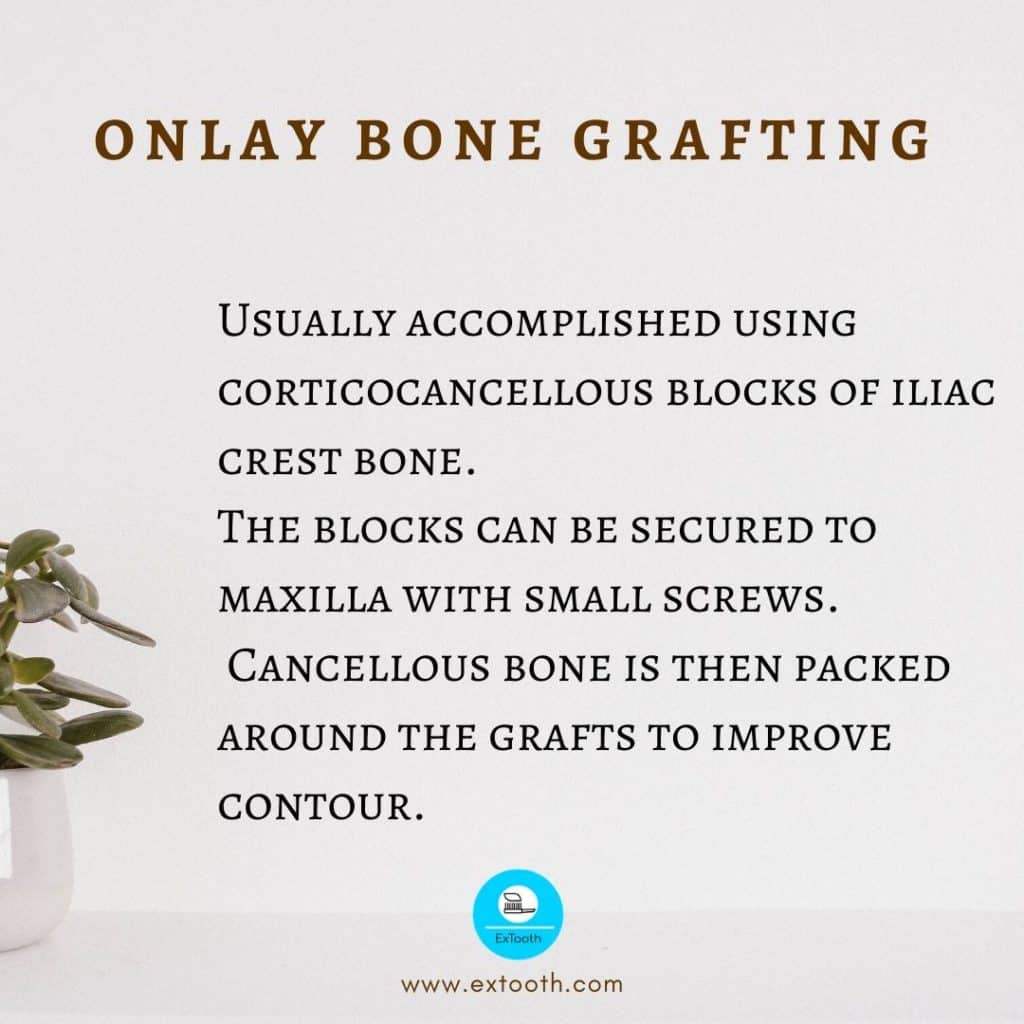
- ONLAY BONE GRAFTING.
- INTERPOSITIONAL BONE GRAFTS.
- MAXILLARY HYDROXYAPATITE
- AUGMENTATION.
MANDIBULAR AUGMENTATION
SUPERIOR BORDER AUGMENTATION
Indicated when severe resorption of mandible results in inadequate height & contour & potential risk of fracture, placement of implants required
Uses autogenous corticocancellous blocks of iliac crest bone.
These pieces of bone are frequently tightened to the mandible with small rigid fixation screws, reducing graft mobility.
MANDIBULAR AUGMENTATION
INFERIOR BORDER AUGMENTATION
Rarely used.
Achieved using iliac crest bone grafts, tightened with rigid fixation
Disadvantage: this technique does not correct the irregularities of denture bearing areas such as superior border changes or disclosed position of mental nerve which results from mandibular atrophy.
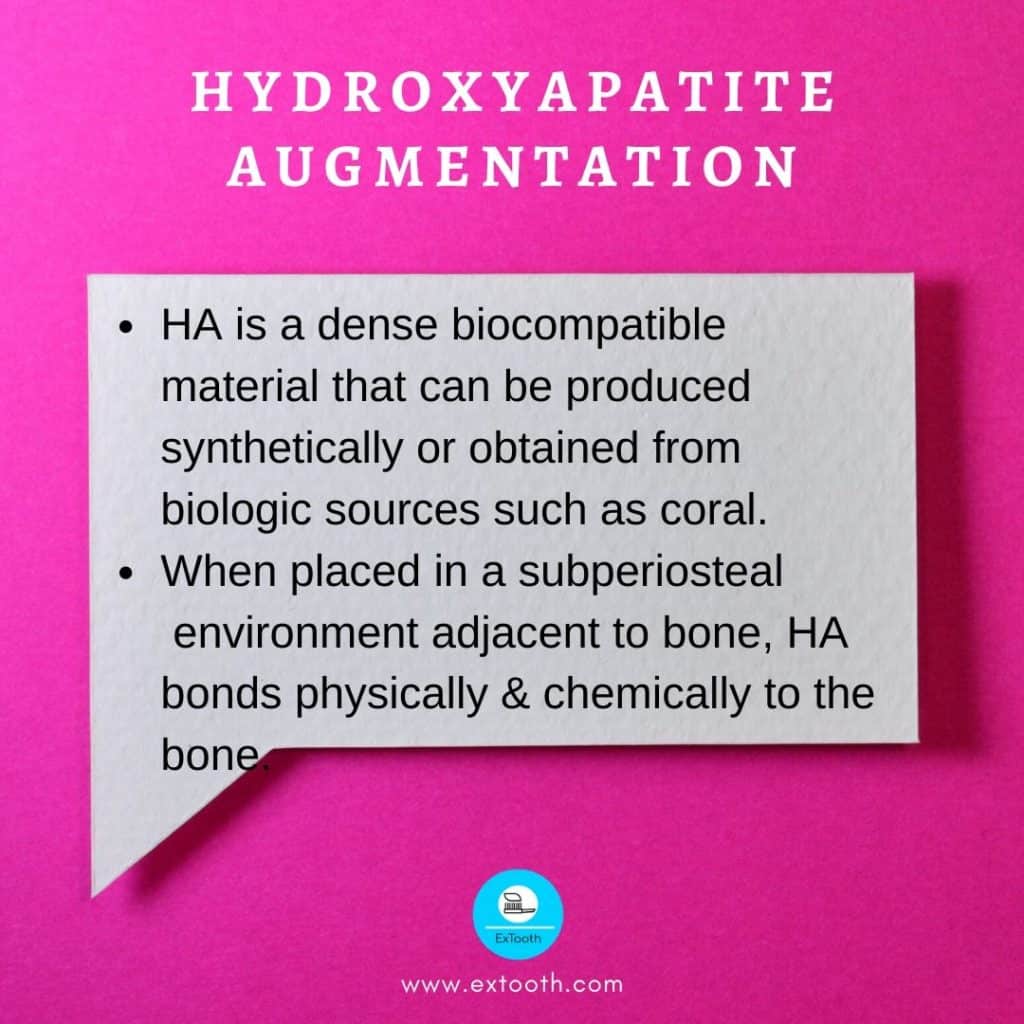
HYDROXYAPATITE AUGMENTATION
ONLAY BONE GRAFTING
INTERPOSITIONAL BONE GRAFTS
It maintains the blood supply to the repositioned portion of the maxilla & generally results in more predictability with less extensive resorption postoperatively.
Indicated in bone deficient maxilla where the palatal vault is found to be adequately formed but the ridge height is insufficient
Advantage: provide stable & predictable results by changing maxillary position in the vertical, anteroposterior & transverse direction.
MAXILLARY HYDROXYAPATITE AUGMENTATION
Eliminates the need for donor site surgery & is easily placed in an outpatient setting
It can be used to contour or eliminate minor ridge irregularities & undercut areas in the maxilla.
Surgical management of Residual ridge resorption
MANDIBULAR RIDGE EXTENSION
- Transpositional flap vestibuloplasty ( Lip Switch)
- Vestibule and floor of the mouth extension procedure
Maxillary ridge extension
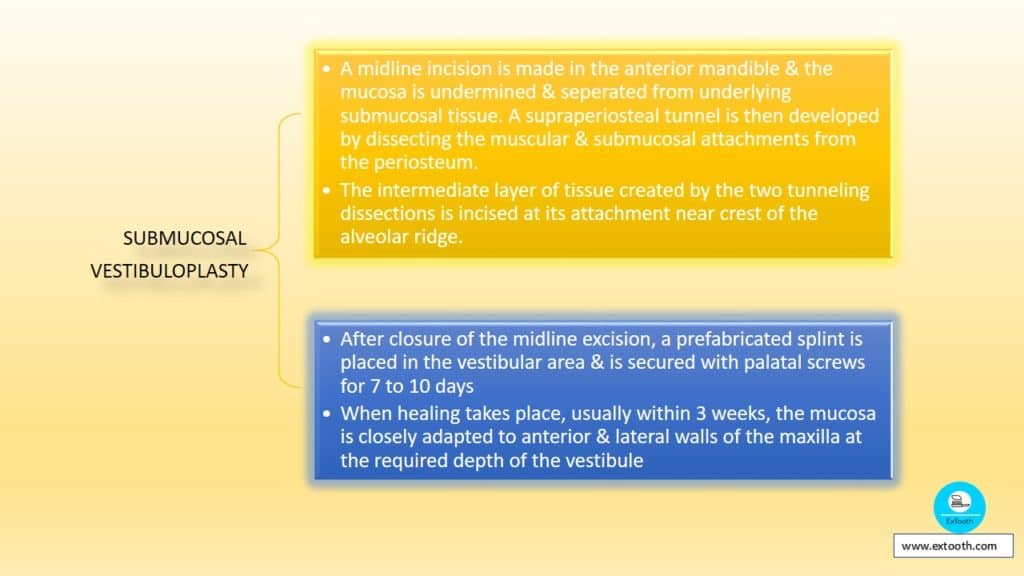
- Submucosal Vestibuloplasty
Vestibuloplatsies are the soft tissue surgeries performed to provide an enlarged area of fixed tissue in primary denture bearing or implant area & to improve extension in the area of denture flanges by removing the dislodging effects of muscle attachments in denture bearing or vestibular areas.
Mandibular ridge extension
Transpositional Flap Vestibuloplasty (Lip Switch)

Vestibule and Floor of the mouth extension procedure
Maxillary Ridge Extension
Submucosal Vestibuloplasty
Overdentures supported by natural tooth roots have been long-standing & integral part of treatment planning.
Now, the overdentures supported by the implants have been introduced.
Although tooth & implant abutment attachment mechanism differs, their prosthetic role is identical. They provide enhanced prosthesis retention & stability, & their influence on adjacent bone levels appears to be similar.
Studies on mandibular overdentures retained by implants have shown that the bone height is maintained in the area where implants were located. However, resorption of the posterior residual ridge was increased when compared with similar sites in the patients treated with implant-supported fixed prostheses.
It seems, therefore, prudent to suggest that younger edentulous patients would benefit from fixed prostheses supported by implants, whereas overdentures should be recommended for elderly edentulous patients.
Prosthetic considerations
The design of the denture should aim at reducing the amount of force on the ridge, thereby reducing residual ridge resorption. They include:
Impression procedures for Residual ridge resorption
Preliminary impression, which is generally overextended
Cast is poured
Resin tray and occlusal rim are made and tried in the mouth
Borders are adjusted so that the lingual flange and sublingual crescent area are in harmony with the resting and active phases of the floor of the mouth in the mandibular arch
The buccal and lingual extensions of the tray are adjusted just short of the reflections of the cheek and lip min the mandibular arch
Peripheral borders are thicker, and peripheral seal should be maintained in the maxillary arch.
Now a stable and non-retentive tray is available
Now a closed mouth or open mouth technique is used to make a master impression
Tissue conditioners are used to make the impression of the resorbed ridge.
There are five special impression techniques for taking an impression of a resorbed ridge.
- Mc Cord and Tyson admixed technique:
Impression compound and green stick compound are mixed in a 3:7 ratio, respectively. Both the materials are put in a hot water bowl at 60-degree Celcius. The mixture is loaded on to edentulous non – perforated tray and impression is taken. - All green technique:
Greenstick material is kneaded at a hot water bath and used to take an impression. One more secondary impression from Zinc oxide eugenol is taken above it. - Closed-mouth functional technique:
A closed mouth impression technique with rims on the denture base described in Winkler. Tissue conditioner is applied to the impression surface three times at every 8- 10 minutes interval. The patient is asked to do functional movements like puffing, blowing, whistling, and smiling during impression in the mouth. A secondary impression with light body elastomeric material is taken above it. - Cocktail technique:
Two pillars or support are made at the posterior region of mandibular denture base opposing maxillary denture base at an increased vertical height. The patient is asked to run tongue against his lips, suck in his cheek, pull in lips, and swallow, keeping the mouth closed. An impression is taken using McCord and Tyson’s admixed technique. - Elastomeric technique:
A secondary impression is taken using a light body elastomeric impression material, usually additional silicon with a tray adhesive.
Conclusion
Resorption of the residual ridges is a natural process. The rate of resorption varies among different individuals and also in the same individual at different times. A dentist should understand the factors causing the residual ridge resorption and treat the patient accordingly using the different treatment options.
WWW.XMC.PL
8 Nov 2020I completely agree with the above comment, the internet is with a doubt growing into the a excellent number of important medium of communication across the globe and its due to sites like this that ideas are spreading so quickly. My best wishes, Alda.