Everyone knows how to make a conventional denture.
What if you get a patient with a systemic disease?
Will you give a conventional denture in the abnormal state?
Lets discuss one by one certain disease and special unusual denture design.
We will discuss it one by one!
OSTEOPETROSIS
= Marble bone disease
= Albers- Schonberg syndrome
= Osteosclerosis Fragilis generalisata
– First described by German Radiologist Heinrich Albers-Schonberg in 1904
– The term introduced by R. G Karshner, in 1922
CLINICAL FEATURES
Two forms of the disease are known
a. Benign dominantly inherited form
b. Malignant recessively inherited form
ORAL FINDINGS
a. delayed eruption of teeth
b. Obliterated medullary spaces of the bones; with osteomyelitis
c. teeth of defective quality, enamel hypoplasia, microscopic dentinal defects, and arrested root development.
LABORATORY FINDINGS
a. acute anemia
b. the serum calcium and phosphorus levels and the alkaline phosphatase level usually remain within normal limits
c. Occasionally there will be a rise in the serum acid phosphatase.
– The lymph nodes, liver, and spleen show extramedullary hematopoiesis and become overworked, enlarged, and incapable of meeting the demands placed on them.
HISTOLOGIC FEATURES
a. osteoblasts are prominent while osteoclasts are seldom seen
b. The trabecular pattern is usually disorganized, and the marrow tissue that is present is usually infiltrated with fibrous tissue.
LITERATURE
Osteopetrosis- Prosthodontic treatment
James D. Woodward, James R Smith and Heinz O Beck
JPD 1976, 35; 6; 608-13
– A 5-year-old girl of Indian parents. One of the three children.
– A distant maternal cousin had a similar condition.
– The patient was small for her age and walked with an unsteady gait.
– She was partially deaf and had lost some of her vision.
– The patient had two maxillary, and two mandibular erupted deciduous central incisors.
– Radiographs showed other unerupted teeth in the maxillae and mandible, but the cortical layer of bone was so dense that it was felt that no more teeth would erupt.
Procedure for denture fabrication
a. Diagnostic impressions in stock pedodontic tray using alginate.
b. Final impression
c. Master casts and denture base using sprinkle on method
d. Inter-arch space in the posterior region was inadequate, and placing both bases would open the vertical dimension. Therefore, since the lower ridge was very firm, only the maxillary occlusion rims and soft wax were used to register centric relation. This method was successful, and an accurate mounting was obtained and subsequently verified.
e. The diminished inter-arch space in the posterior part of the mouth required that the lower base be cut back several millimeters from the retromolar pad.
f. Only six anterior teeth on each denture and a narrow, flat block of acrylic resin to serve for the posterior occlusion could be utilized.
g. The four central incisors were used as support for overlay type of dentures.
h. Pedodontic – size acrylic resin teeth were selected
i. The dentures were processed and finished in acrylic resin except for a small region resting on the retained teeth, which was processed in soft acrylic resin,
j. The patient adapted well to the dentures. Her mastication probably was not improved, but she was very happy to have her new teeth.
CLEIDOCRANIAL DYSOSTOSIS
= Osteodental dysplasia
= Mutational dysostosis
=Marie- Sainton syndrome
– a genetic disorder affecting the bones and teeth
– transmission as true Mendelian dominant factor of high penetration
– solitary case- mutation
– The first reported in medical literature in 1765. Marie and Sainton gave the name “Cleidocranial Dysostosis” in 1989.
CLINICAL FEATURES
- General physical findings–
- The closure of the fontanelles and sutures in the cranium is delayed
- Frontal, parietal and occipital bossing
- Brachycephalic
- The sagittal suture is characteristically depressed giving the skull a flat appearance
- Paranasal sinuses are underdeveloped and narrow
- The clavicles may be hypoplastic or absent- usually results in a long neck and narrow, sloping shoulders that permit the individual to bring the shoulders together in front of the chest.
- Have little loss of function and may be muscular and active.
- Deviations from normal in other bones may or may not be present.
- Individuals may be of short stature
- The mentality in these patients is generally normal
- Dental findings–
- The maxillae are underdeveloped, while the growth of the mandible is normal.
- High, narrow arched palate and cleft palate are common.
- Over closure- prognathic appearance
- The deciduous teeth erupt normally, all the permanent teeth generally lose eruption stimulus and remain embedded.
- Embedded supernumerary teeth
- Non- succedaneous teeth may erupt normally.
TREATMENT
Since the bony changes are not disabling, the dentist is often the first person to diagnose. Results of some kind have been reported only after prolonged orthodontic treatment. Acceleration of tooth eruption by orthodontic means is difficult, although the roots do not seem to ankylose. In most patients, orthodontic treatment has been concentrated on the eruption of a few chosen teeth for abutments for RPD or FPD. Generally, the prognosis of orthodontic treatment is poor, so the prosthodontic treatment is the treatment of choice.
LITERATURE
Cleidocranial dysostosis- A prosthodontic problem
Ellsworth Kelly and Roy Y Nakamoto
JPD 1974,31;5;518-26
Prosthodontics treatment presents a unique opportunity in rehabilitation. Increasing the occlusal vertical dimension, building out the maxillae, and establishing a functional occlusion dramatically improves appearance, function, and sometimes speech. With a vastly improved appearance, the patient often undergoes marked improvement in mental outlook and personality.
The ridges for the support of denture bases in patients with cleidocranial dysostosis are generally full and rounded because of the embedded teeth they contain and cannot be rightly called “edentulous ridges”. However, the embedded teeth are not stimulated by the pressures from denture bases. They may be exposed by bone resorption. No reports advocate their removal before treatment.
Patient reports:
I. A 31-year-old Caucasians man, somewhat under normal height, who had a history of asthma and poliomyelitis without sequelae. He had retained his entire deciduous dentition except for the upper left and lower right second molars. The lower first and second permanent had erupted and were in normal position in the dental arch. The upper right first and second and upper left second permanent molars have erupted in normal position. A class I malocclusion existed because of the underdeveloped maxillae. The occlusal vertical dimension was so short that there were about 8mm of inter-occlusal distance at-rest position. Radiographs revealed many embedded teeth with a large dentigerous cyst involving the left maxilla.
The clavicles were absent, and there were bossing of the frontal bones and slight depression of the median suture.
ECTODERMAL DYSPLASIA
= Hereditary hypohydrotic (anhydrotic) ectodermal dysplasia; Christ-Siemens- Touraine syndrome
– Characterized by a congenital dysplasia of one or more ectodermal structures and their accessory appendages, manifested primarily by hypohydrosis, hypotrichosis, and hypodontia
– The most common type of ectodermal dysplasia.
– The majority of cases are X-linked recessive Mendelian character.
Clinical features
a. Patients usually exhibit a soft, smooth thin, dry skin with the partial or complete absence of sweat glands ( hyperpyrexia)
b. The sebaceous glands and hair follicles are often defective or absent.
c. The hair of the scalp and eyebrows tend to be fine, scanty, and blonde and resembles lanugo. The mustache and beard are usually normal in appearance.
d. The bridge of the nose is depressed, the supraorbital ridges and frontal bosses are pronounced, and the lips protuberant.
Oral manifestation
a. Anodontia or Oligodontia
b. Even in complete anodontia, the growth of the jaws is not impaired.
c. Since there is no alveolar process, there is a reduction in the normal vertical dimension resulting in protuberant lips.
d. A palatal arch is frequently high, and a palatal cleft may be present.
e. Salivary glands (major and intraoral accessory) are sometimes hypoplastic with resulting xerostomia.
f. Lips may be dry and cracked.
g. Hypoplasia of nasal and pharyngeal mucous glands can lead to chronic rhinitis &/or pharyngitis, sometimes with associated dysphagia and hoarseness.
Treatment
a. There is no treatment for the condition
b. from a dental standpoint, partial or full dentures should be constructed for both functional and cosmetic purposes.
c. an unusual denture may be used even in relatively young patients, but they must be reconstructed periodically as the jaws continue to grow.
LITERATURE
X- linked hypohydrotic ectodermal dysplasia- an unusual prosthetic problem
C. J Nortje, A.G Farman, C. J Thomas and G J J Watermeyer.
JPD 1978, vol 40 no.2 137-42.
Hypohydrotic ectodermal dysplasia (X-linked) is a form of ectodermal dysplasia that affects only males severely, while female heterozygote shows only minor defects. The first description of this condition has been attributed to Widerburn by Darwin, but the term hereditary anhidrotic ectodermal dysplasia was introduced by Weech.
Treatment of a patient:
– A caucasian boy of European extraction aged 4, with typical features of hypohidrotic ectodermal dysplasia.
– Intraoral examination showed the only erupted teeth to be cone-shaped deciduous maxillary incisor teeth.
– Radiographs: permanent equivalents of deciduous incisors
– Mother seemed normal with blonde hair, but examination revealed partial anodontia.
– Prosthetic management of the child:
a. diagnostic impressions using irreversible hydrocolloid
b. The casts showed underdeveloped maxilla and mandible that would offer little resistance to movement in the lateral and anteroposterior direction.
c. The existing teeth in the premaxilla could be used to improve stability if a complete overdenture were constructed.
d. Custom acrylic trays, jaw relation, and trial
e. Tooth position was dependent upon two remaining natural teeth, which were precisely overlaid with pedodontic –size acrylic resin substitutes.
– Prosthetic treatment is of immense psychological benefit to the patient.
Fixed rehabilitation of a patient with hypohidrotic ectodermal dysplasia using Zygomatic implants
Valencia university medical and dental school and university of Valencia
Oral surg Oral med Oral pathol Oral radiol Endod 2004;98:161-5
Clinical Case:
– A 29-year-old male with typical features of the disease
– Intraoral- total upper and partial lower edentulism
– OPG and CT revealed extreme maxillary atrophy with little remnant bone.
– Management: fixed maxillary rehabilitation over implants including 2 transzygomatic implants, with the placement of inferior overdentures on the remaining mandibular teeth.
– Surgery was carried out under general anesthesia
– A supracrestal incision was made from one tuberosity to another, with distal extensions. The beds were prepared in the anterior zone with the help of osteodialtors.
– Three implants- 12mm length; 4.1 mm diameter were positioned. Two in the remnant bone of the canine processes and 1 in the cortical component in the nasopalatal duct.
– Two zygomatic implants were in the area of missing teeth 3 and 14, measuring 35mm in length, by means of the sinus slot technique
– Analgesics and antibiotics were prescribed and monitored postoperatively after 7, 14, 30, and 60 days.
– After six months, a complete upper prosthesis was screwed onto the implants, and the lower overdentures were placed. The patient showed great improvement in function and self-esteem.
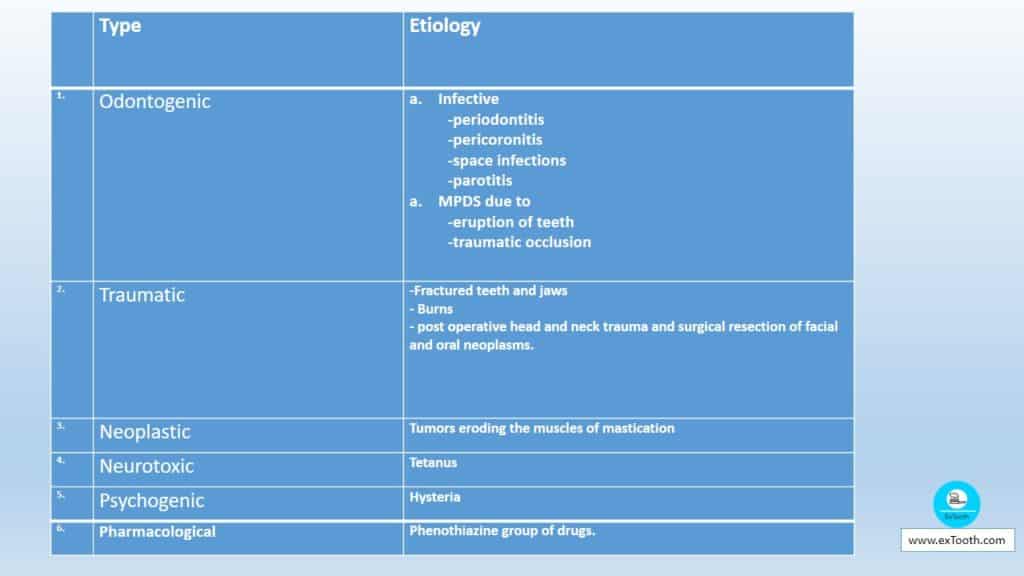
MICROSTOMIA
Tonic contraction of the muscles of mastication, causing an inability to open the mouth to the normal extent, is called trismus. The condition may occur in
1. Mouth infections
2. encephalitis
3. Inflammation of the salivary glands.
4. Tetanus
5. Surgical injuries ( head and neck tumors)
6. head and neck radiation
7. reflex spasm
8. micro invasion of the muscles of mastication
9. connective tissue disease
10. fibrosis of masticatory muscles
11. oral submucous fibrosis
In patients with oral malignancy, post-treatment trismus is more commonly found in patients with mandibular tumors than with maxillary tumors. Trismus can be a significant problem for patients who need dental treatment. However, clinical management of the problems associated with providing a dental prosthesis for the patients with trismus is not well reported. The clinical management of trismus includes surgery, usage of opening devices, and modification of denture designs.
OSMF: It is a gradually increasing chronic fibrotic condition of the mouth and oropharynx, characterized by fibroelastic change and inflammation of the mucosa, leading to a gradual failure to open the mouth, swallow or talk.
LITERATURE
1. Treatment of an edentulous patient with surgically induced microstomia:
A clinical report
Laith Abd Al-Hadi and Hana Abbas
JPD 2002, vol 87, 423-6
A 50-year-old female with congenital bilateral Bell’s palsy and loss orbicularis, with few remaining periodontally involved maxillary teeth and edentulous mandible, was referred for treatment. The patient was previously treated with segmental osteotomies and a facial sling, resulting in limited mouth opening. The patient’s lower lip was supported by a sling to keep the mouth closed and to prevent saliva pooling and drooping of lips. The sling made any attempt to extend the lip impossible. The mandibular movement was limited to simple opening, and closing and eating and speaking abilities were impaired.
– the mandibular ridge was divided into three segments for preliminary impression and the impression was poured in plaster of paris.
– Custom acrylic trays were fabricated. Their handles, made of 1 mm generic stainless steel wire, were manipulated to permit placement and stabilization of each tray on the corresponding segment within the available space.
– Light body vinyl polysiloxane was used to make the final impression after the patient rinsed her mouth with a sodium bicarbonate solution to reduce the effect of mucin on the impression. The three tray sections were placed in the mouth, and a soft modeling compound was used to index and stabilize the segments.
– After the impressions were made, the modeling compound was chilled and removed. The impression tray segments then were removed and reassembled, and the cast poured in stone.
– Sectional trays were fabricated, and a ZOE impression made to correct any defects in the previous impression.
– On the final working cast, two layers of wax were adapted to each side of the arch up to the midline, where they were separated by 2mm. It was processed to obtain the denture bases.
– Jaw relations were obtained and transferred to a simple hinge articulator
– The try-in sectional denture was assessed to check jaw relationships and tooth arrangement.
– To attach the two segments, horizontal dovetails were prepared on the labial and lingual sides of the segments. For additional retention, two pins were inserted into two prepared holes in the top segment, which held the 4 anterior teeth. The patient found this arrangement difficult to handle.
– To simplify insertion and stabilization, vertical dovetails were prepared on the labial and lingual surfaces of the denture segments. They were grooved on the recipient denture section to permit vertical insertion movement only.
– The two parts were reassembled, and the matrix was waxed, flasked, and processed with 0.02 mm thick plastic separator. The completed denture was finished and polished as 1 unit to prevent possible distortion of the resin.
– The denture was inserted, and pressure disclosing paste was used to refine the tissue surface.
– To facilitate the disengagement of the 2 denture segments, a notch was prepared on the matrix. The patient expressed satisfaction with this method of placement.
Prosthetic restoration in microstomia
B Conroy and M Reitzik
JPD 1971,26;3 324-7
The provision of satisfactory dentures for patients with a reduced stomal inlet has always been a problem. The smallest diameter of a fully retentive maxillary denture is often much larger than the greatest diameter of the mouth opening, and the most common compromise is to wear a RPD for appearance. Even if a complete maxillary denture can be inserted into the mouth, it further reduces the stomal inlet, and the insertion of mandibular denture is made impossible.
PATIENT REPORT:
– F L, 46 years, sustained burn injuries when the petrol tanker he was traveling in was torpedoed.
– Facial scarring reduced the width of the mouth and poor oral hygiene.
– Treatment procedure:
a. A clearance and alveolectomy were performed under GA
b. A sectional impression of the maxillary ridge with impression plastic
c. Chill; trim to midline
d. Coat with petroleum jelly
e. Reposition on the maxillary ridge
f. Make a sectional impression of the other half.
g. Same procedure for the mandibular arch
h. Pour stone casts
i. Make a maxillary acrylic resin base covering posterior two-thirds of the cast.
j. Incorporate a midline stainless steel hinge as far back as is possible on the acrylic resin base
k. Similarly, make a mandibular acrylic resin base incorporating the stainless steel hinge anterolingually
l. Take maxillary and mandibular final impressions with ZOE paste inside the prepared hinged bases.
m. Pour stone casts into final impression
n. Separate the hinged trays from the casts
o. Readapt, the hinged trays to the stone, casts by relining
p. Establish jaw relation records using posterior teeth in maxillary baseplates
q. Mount the baseplates in an instrument to the established jaw relation records
r. Arrange the teeth and check to confirm the relation
s. Complete the final wax-ups
t. Use a surveyor and cutting instrument to make recessed channels palatally and between 65/56 in the finished maxillary wax-up to accommodate a retaining chrome-cobalt framework
u. Use cutting instruments and a model surveyor to prepare the recess on the lingual side of the mandibular denture and between premolars for the mandibular framework
v. Process and finish the maxillary and mandibular set-ups in acrylic resin
w. Make an alginate impression of the anterior one-third of the maxilla and prepared recessed groove in the palate
x. Make an alginate impression of the prepared lingual section of the mandibular denture
y. Pour casts from the impressions
z. Cast and finish the retaining frame and grid retention for the maxillary and anterior teeth in a chrome-cobalt alloy
- Process anterior teeth to the chrome-cobalt alloy framework completing the restoration
- Cast and finish the mandibular lingual stiffening frame in chrome-cobalt alloy.
A sectional complete denture for a patient with microstomia
J Fraser McCord, Kenneth W Tyson and Ian S Blair
Jpd 1989; 61;645-7
The patient was a 50-year-old edentulous woman who developed constricted mouth opening following surgery for a carcinoma in the left cheek followed by radiation therapy.
A maxillary sectional impression tray was made, and a master cast poured. A duplicate cast was relieved over the incisive papilla and palatal raphe with 1.5 mm tinfoil. The procedure was similar to the try-in of dentures.
The completed sectional denture was designed in two halves, with the left side fitting into a beveled recess on the right side to give a more accurate location. Both halves were joined rigidly by a stainless steel post that inserted into three tubes within the complete denture palate. The post, which was removable, was attached to the right maxillary incisor, which served both as a tooth and as a handle for the post.
A simplified technique for prosthetic treatment of microstomia in a patient with scleroderma : A case report
Laith Abd Al- Hadi
QI 1994 ;25 ;8; 531-3
Case report:
– 60-year-old woman, a patient of scleroderma
– Intraoral examination revealed 7/47
– Anterior maxillary ridge markedly resorbed and covered with scar tissue
– Tuberosities enlarged.
– Undercuts labially and buccally.’
– Mandibular edentulous ridge irregularly resorbed.
– The case was treated with a partial maxillary denture in 3 articulated pieces and one-piece mandibular complete denture.
Flexible denture flanges for patients exhibiting undercut tuberosities and reduced width of the buccal vestibule: A clinical report
Leonard Garth Lowe
JPD 2004; 92; 128- 31
Unilateral or bilateral undercuts on the buccal aspect of the maxillary tuberosity are frequently encountered and may complicate the successful fabrication of a complete denture. Management in these situations includes alteration of the denture bearing area, the adaptation of the denture base, careful planning of the path of insertion, and the use of resilient lining materials.
This clinical report describes an alternative denture design in which optimal flange height and thickness can be achieved in situations where the maxillary tuberosities are bilaterally undercut and bulbous, and the vestibular width is limited, using a resilient liner material for the flange. The design allows the attainment of a border seal and prevention of anatomical dislodgement by the coronoid process. This design is especially useful where surgical intervention is contraindicated.
The hollow denture: An alternative treatment for atrophic maxillae
LaDeane Fattore, Louis Fine, and David C Edmonds
JPD 1988; 59; 4; 512-6
Technique:
– Make a clear heat-cured baseplate to fit the anatomical portion of the cast
– Construct occlusion rims
– Jaw relation, mounting and teeth arrangement
– Invest
– Dewaxing
– To the cool flask, adapt 2mm thick baseplate wax to the tooth side of the flask. Avoid creating undercuts in the wax even if it is necessary.
– Put the halves of the flask collectively with a plastic sheet separating them. Ensure complete closure
– Place a similar flask lid on the upper half with the baseplate wax and the teeth and pour a cast in stone.
– Heat out, clear and apply tin foil substitute as routine
– Pack and cure
– Cool, divide the flask and delicately extract any flash but do not deflask
– Both halves of the initial flask now hold a processed acrylic resin shell. Adapt the two halves of the flask together and eliminate any acrylic resin that conflicts with complete flask closing.
– Make a ‘rope’ of doughy resin and adapt it around the border, trial pack closes the flask and cure.
– Cool the flask before deflasking.
– Finish and polish.
CLEFT PALATE PROSTHESIS
Perhaps more has been written about cleft palate prosthesis than any other unusual denture, but there is little systematic knowledge regarding the retention of complete dentures for the cleft palate patient.
Classification
Class I – cleft of soft palate alone
Class II – cleft of soft and hard palate in the midline.
Class III- cleft of soft and hard palate that continues on one side of the premaxillary area (with or without cleft lip of the same side).
Class IV – cleft of the soft and hard palate going through the alveolar ridge on both sides, leaving a free premaxilla in between. It may or may not be associated with a bilateral cleft lip.
Problems:
· Inferior portion of the Vomer may be deficient.
· Chronic inflammation of the inferior turbinates.
· Constant swelling of the turbinates may encourage chronic sinusitis.
· Inadequate action of the soft palate may direct small food particles into the Eustachian tubes located in the nasopharynx. Bacteria then multiply in this substrate and cause inflammation, which, progressing up the tube, may lead to middle ear diseases.
· Limited speech capability.
Treatment
I. Surgical – the most preferred form of treatment
II. Prosthetic
PROSTHETIC TREATMENT
The patient with an unrepaired palatal cleft and is also edentulous will find it difficult to wear a complete denture obturator. Those forces which ordinarily influence the retention of the dentures such as cohesion, adhesion, atmospheric pressure, and peripheral seal are still active, but their quantitative effect is less. None the less, the unusual denture must be designed to take maximum advantage of all retentive aids.
Impression for the unusual denture:
· It is always advisable to obtain a preliminary impression in alginate material. The chosen tray should have at least 3 to 4 mm space between it and the tissues.
· Soft utility wax may be placed on the tray so that most of the impression material is confined to the mucosal bearing area and not forced into the cleft.
· When the tray is filled, the tray is under-loaded in the cleft area. This is true in unrepaired clefts and also in perforations, which may result from tissue breakdown in a previously repaired cleft.
· In cases of class II and III clefts, the maxillary arch should be examined carefully for all possible openings like small perforations in the mucobuccal fold.
· A gauze patch (1 sq cm) may be used to prevent the impression material from entering the defect. In large openings, wax damming on the tray and practice of under loading the tray in that area will almost always prevent impression material from entering the nose.
· Peripheral seal:
a. When the preliminary impression has been poured, an acrylic tray for the final impression is made. The compound for a peripheral seal is handled differently.
b. The seal in class II cases is started with the buccal seal from the frenum along the right side of the denture, continued through the right hamular notch, running medially at the post dam area until it reaches 3 to 5 mm from the cleft edge. Here it turns forward and runs along 3 to 5mm from the cleft edge, turns across the anterior limit of the cleft, runs back against the opposite edge, and turns at the post dam area to run laterally toward the hamular notch. It then courses through the notch to the buccal periphery and along the latter to complete the seal anteriorly at the anterior frenum.
c. Classes III and IV are handled similarly except that the cleft, which continues through the alveolus, would break the total seal. This imposes the necessity of sealing two separate chambers instead of one. A separate peripheral seal must be created on one side of the cleft and another on the other side.
d. The available surface area is relative
e. The final impression is handled in a manner similar to that used for the normal denture except that, again, the tray is underloaded in the area of the opening.
f. The final impression can be sealed by scraping the cast an appropriate width and depth in the areas where muscle trimming is not possible.
g. Vertical dimension, centric relation, and tooth arrangement are similar to conventional techniques.
· Pharyngeal section:
- Usually added after several weeks of successful use of the denture
- Three types of obturator
i. Hinged (Olinger 1952- metal hinge adds weight)
ii. Fixed type
iii. Meatus obturator (Schalit 1946- directed almost 90 degrees upward to reach the roof of the nasopharynx)
- If the patient cannot tolerate the pharyngeal section well, it is better to remove it as it is better to supply one lost function and not another than to supply none.
MEATUS OBTURATOR
Requires no muscle trimming, and results can be ascertained immediately. It is formed by placing a bulk of compound on the posterior section of the denture in such a manner that the mass is directed upward to the roof of the nasopharynx. This bulk is initially smaller than the space it must occupy; it is gradually enlarged until the nasopharyngeal tissues are contacted.
If placed properly in an anteroposterior direction, this compound mass should include an impression of the vomer bone, the lower turbinates, and perhaps the Eustachian tube opening.
– the pharyngeal section of the appliance affects mainly the nasality
– provide immediate and dramatic results
– Results are uniformly better if obturators are directed as high up on the pharyngeal wall as possible.
Muscle trimming of the pharyngeal section is by asking the patient to swallow, bend the head far forward, backward, and twist it from side to side.
The prognosis of the prosthesis is directly dependent on the weight. The lighter the appliance, the greater the chance of success.
TO MAKE AN OBTURATOR OR NOT
To make such a decision, it is convenient to divide the patients into three classes
a. Those not suitable for surgical closure of the soft
Palate
b. Those who have grown up without any surgical
Treatment
c. Those who have had unsuccessful surgical treatment
– Class a patients should be fitted with an obturator as soon as they are old enough to allow it remain in place ( usually between 2 to 3 years)
– Class b
1. no treatment at all
2. denture carrying an obturator
3. surgical repair
– Class c – it is important to determine if the soft palate is competent. Two valuable tests to determine the bunching up action are-
1. Snoring test- snoring results from drawing air in through the nose and by its passage to the lungs forcefully separating the raised soft palate from the pharyngeal wall. The air passes in a series of short puffs, causing the soft palate to vibrate, producing the snoring sound. If the soft palate is incapable of making firm contact with the pharynx, snoring is impossible.
2. a lateral cephalograph taken after several drops of Barium solution have been introduced into each nostril while the individual is lying down and head gently moved from side to side to spread the Barium over the palate and pharynx. The exposure should be made while the patient is making the action of sounding a prolonged “p” but without actually parting the lips. This will cause the soft palate to rise to its high level if it is capable of so doing.
LITERATURE
1. Prosthodontic considerations in the management of surgically compromised cleft palate patients
Robert E McKinstry, Mohamed A Aramany,
JPD 1984; 53; 827-31
Cleft palate surgery should restore functioning anatomy that improves speech, oronasopharyngeal physiology, and esthetics without interfering with form and function. When surgical results are less than desirable, prosthodontics management may be necessary as in patients with –
1. surgically redivided palates
2. nonfunctional pharyngeal flaps
3. large or multiple perforations
4. Palatopharyngeal insufficiency and/or incompetence after surgical repair.
Surgical re-division of the palate:
Necessary if surgery results in –
a. multiple perforations in the palate usually along the suture line
b. Extensive cleft areas separated by bands of soft tissue.
c. A heavily scarred palatal vault that restricts oral space and necessitates placement of prosthesis at a level inconsistent with comfort and efficiency.
d. Limited mobility of palatal muscles, which may displace a speech aid prosthesis.
– The role of the levator veli palatini muscles must be considered in patients with surgically redivided palates.
– Surgical redivision should not include the removal of levator muscles.
– When palatopharyngeal insufficiency or incompetence persists after the surgical repair of the palate, the prosthodontist should consider the use of videofluroscopy and nasal and oral endoscopy in constructing a prosthesis that permits successful palatopharyngeal closure.
– In children with surgically redivided palates stainless steel bands may be used in the construction of speech aid prosthesis, whereas those for adults are fabricated using chrome- cobalt partial denture framework.
Nonfunctional pharyngeal flaps:
In the surgical procedure, a unipedicle soft tissue flap is elevated from the posterior pharyngeal wall. It can be inferiorly or superiorly based, depending on the needs of the patient and the preference of the surgeon. While the proximal end of the flap remains attached to the pharyngeal wall, the distal end is connected to the residual palate to separate the oropharynx from the nasopharynx. On each side of the flap, lateral openings permit nasal breathing, nasal drainage and nasalization for indicated speech sounds. The flap must be wide enough and at the proper superior inferior level to permit closure. However, the flap must not occlude passage for nasal breathing.
If the flap is too narrow, an obturator is an easiest and most reliable procedure to reduce the size of the lateral ports.
Soft palate perforations:
Presents failure of surgical closure. The most common causes are-
1. Inadequate approximation of opposing surgical surfaces.
2. closure under tension
3. infection
4. improper suturing.
5. traumatic disruption of the healing wound.
The symptoms associated with these perforations vary with size and location. The location of the perforation also influences prosthodontics management. If the perforation is located close to the area of maximum soft palate elevation, placement of the pharyngeal section through the perforation with the soft palate remaining inferior to the speech aid prosthesis is less than advantageous. Prosthodontic treatment may be the initial treatment of choice in patients who develop large postsurgical fistulae. These patients may also be considered for redivision of the palate to permit better prosthodontics management.
Palatopharyngeal insufficiency and incompetence after surgical repair:
It can be managed surgically by palatal lengthening procedures, posterior pharyngeal wall implants, temporal muscle- fascial slings, pharyngoplasties and pharyngeal flaps. When surgical repair must be deferred temporarily or permanently, a speech aid prosthesis may be used.
The soft palate section of the prosthesis must often be placed inferior to the obturator to circumvent the soft palate and position of the obturator at the proper superior –inferior level. This type of prosthesis may also be used in patients with neurologic deficits secondary to repeated surgical procedures.
Prosthetic reconstruction following resection of the hard and soft palate
Mohammed A Aramany and Eugene N Myers
JPD 1978; 40; 174-8
Defects may be classified into the following categories:
I. Total resection of the soft palate, retaining a part of the hard palate.
– Soft palate is totally removed
– The function of the superior constrictor of pharynx remains intact.
– This is similar to the unrepaired congenital cleft of the palate.
II. Median resection of the palate.
– The resection may involve parts of the hard and soft palate.
– The levators, tensor, uvula, palatoglossus and palatopharyngeus muscles are left functionally intact.
– The normal functional movement of the palate will take place on eliciting the velopharyngeal mechanism, whereas the presence of the defect will make this movement functionally inadequate.
– The anterior margin of the defect is not mobile, whereas the posterior aspect of the defect will move superiorly and posteriorly, increasing the size of the oronasal communication.
III. Lateral resection involving approximately half of the soft palate.
– the clearance is usually to give adequate surgical margins
– The muscles of the other half are left intact.
– The soft palate tends to elevate more laterally toward the normal side and more superiorly, since there is no limiting action of the other side muscles.
Prosthetic treatment of the soft palate:
Three different obturator designs are used to restore the soft palate.
I. Prosthesis for total soft palate resection
– A speech aid prosthesis extending posteriorly from the base of the prosthesis into the pharyngeal region separates the oropharynx from the nasopharynx.
– The success of this prosthesis is dependent on the action of the superior constrictor muscle of the pharynx separating the two cavities during speech and swallowing.
– At rest, there is a space around the pharyngeal part of the prosthesis to affect nasal breathing.
II. Prosthesis for median palatal defect
– the functional defect is confined to the soft palate. The velopharyngeal mechanism is intact.
– The extension from the parent prothesis passes through the soft palate defect to produce and oronasal seal.
– The posterior extension of the prosthesis does not extend to the posterior or lateral pharyngeal wall.
– The velar extension passes through the defect, and at rest position a space is present between the prosthesis and the posterior margin of the defect.
– During speech or swallowing, the levator and tensor muscles contract and the margins of the defect elevate to separate the oropharynx from the nasopharynx.
III.Prosthesis for lateral soft palate defects
– The level of the muscular activity of the remaining segment of the soft palate is considerably higher in the pharyngeal region than in the intact palate.
– If the defect is small, velopharyngeal closure may be effected without the help of a prosthesis
– If the defect is large or the patient is unable to develop compensatory movement, a retrovelar speech aid is constructed.
– A pharyngeal extension from the base of the prosthesis passes through the defect and fills the potential space behind the remaining segment of the soft palate.
– Velopharyngeal closure is attained by the levator action of the remaining soft palate and the contraction of the pharyngeal muscles against the pharyngeal extension of the prosthesis.
– If the patient regains ability of velopharyngeal closure, a program of gradual reduction of the pharyngeal extension is followed.
– Rehabilitation may also be made more complex if partial segmental resection of the mandible at the angle has been included in the resection. A guiding mandibular prosthesis may need to be constructed along with the maxillary deviation.
– Patients with lateral soft palate defects are the most difficult to manage prosthetically.
– The large regional pedicle flaps currently utilized for reconstruction provide static rather than dynamic replacement for the oropharyngeal musculature. This eliminates the pharyngeal component of velopharyngeal closure mechanism against the retrovelar speech aid.
– Patient acceptance of the prosthesis is the key to success in these conditions.
OROFACIAL DYSKINESIA
There are a number of movement disorders which involve the oral, facial and cervical musculature. One of these, orofacial dyskinesia, is characterized by severe involuntary dystonic movements of these structures. Among the purposeless movements seen are lip smacking, protrusion of the tongue and mandible, grimacing and clonic spasm of the muscles of the anterior aspect of the neck, chest and shoulder. This dyskinesia may appear as the sole abnormality, or it may be associated with torticollis or with generalized dystonia, as in musculoram deformans. It is more commonly seen in the elderly than in the younger ones.
LITERATURE:
1.Orofacial dyskineia: Effective prosthetic therapy
Howard D Sutcher, Robert A Beatty and Robert B Underwood
JPD 1973 vol 30 no.3 252-62
Patient report:
The patient was a 45-year-old Caucasian woman who had worn dentures for many years. Her medical history was negative. The onset of orofacial dyskinesia was gradual and progressive and the symptoms had persisted for one year. Her speech was slurred and she exhibited severe, continuous, involuntary dystonic movements of the oral, facial and cervical muscles. Her tremulous tongue seemed too large for the oral cavity. It protruded from the mouth, lacked all fine movements and was constantly moving in a purposeless fashion. The patient was able to touch her denture teeth together but was unable to hold them together for more than a few seconds and could not clench.
– The existing occlusal relationships were improved by adding a layer of cold curing resin to the upper denture and the patient guided into bite in the rubbery stage of the material.
– It formed a channel in which the lower denture would fit.
– When the dentures were approximated, the labial portion of the lower denture was almost completely covered by the occlusal splint.
– There was dramatic improvement in the dyskinetic movements
– The original splint had to be altered or remade many times over the several months.
– Relapse of the condition occurred within 30 seconds of removal of the dentures
– Once an acceptable craniomandibular relationship was established, as evidenced by the disappearance of symptoms, the depth of the splint was reduced. Ultimately, indentations of less than 1 mm appeared to be sufficient to maintain the most acceptable jaw relationship.
– The terminal hinge position was resisted by the mandible even after the symptoms subsided.
– NEW DENTURES:
a. Borders of existing dentures relined with cold-curing resin
b. Fit improved with soft liners- served as final impression
c. Cast and splint mounted as one unit.
– The new dentures included certain unusual modifications that helped to guide the patient’s mandible to her centric occlusion position.
1. 33 degree posterior teeth, balanced only in centric occlusion
2. cuspids in a deep vertical overlap with no horizontal freedom ( locked cuspids)
3. a modified bite plane behind the maxillary incisors into which the mandibular incisors fit, and
4. Guiding ramps on the posterior areas of the dentures.
– These ramps appear to be the most effective modification. They consist of triangular female slots in the retromolar regions of the mandibular denture and triangular male inserts in the tuberosity regions in the maxillary denture.
– Since the arc of closure in the posterior regions is smaller than that in the anterior regions, the guiding ramps can be constructed so that they are active with the mouth open rather widely. Thus, the ramps are available to signal proprioceptive cues at almost any time through a large range of vertical jaw movement.
– Repeated reducing and tightening of the ramps evolved in their optimal fit.
Prosthodontic management of a patient with neurological disorders after the resection of an acoustic neuroma:
JPD 2002;87; 419-22.
– Neurinoma is a slow growing benign tumor that originates from Schwann cells.
– The acoustic neurinoma originates just inside the internal auditory meatus
– The most common resulting neurological disorders are unilateral facial paralysis of the peripheral type, unilateral facial hypalgesia, ipsilateral cerebellar ataxia, dysphonia, dysarthria and dysphagia. The increased intracranial pressure also causes headaches and vomiting.
– The 85 year old man presented with cerebellar ataxia and unilateral disorders of V, VI, VII, VIII, IX, X and XI nerves.
– After a long recovery period he was able to perform daily hygiene functions including those related to oral hygiene.
– An extra- oral examination revealed a considerable right sided facial weakness, loss of sensation of skin on the affected side and a reproducible contralateral deviation of the mandible on opening but no signs or symptoms of angular stomatitis.
– An intra oral clinical examination revealed a completely edentulous oral cavity with well rounded residual ridges, deviation of the tongue during rest and on protrusion, impaired deglutition and lack of oral and pharyngeal sensation on the affected side. There were no signs or symptoms of salivary hypofunction.
– The patient’s chief complaint was impaired mastication due to inadequate retention and stability of his existing dentures.
– A replacement maxillary denture combined with mandibular denture placed in neutral zone was selected as the treatment of choice .
– Initial and final impressions were made using standard techniques making sure to remove any excess material in the posterior palatal seal area immediately.
– Maxillary occlusion rims were trimmed to meet the esthetic needs of the patient ; paralyzed side being carefully retracted to create symmetry.
– A thick mixture of tissue conditioning material was adapted to the top of the mandibular record base with slightly under extended borders and shaped like an occlusal rim.
– The record base was placed in the mouth and the patient asked to sip a little water, swallow and relax; count from 1 to 10 and attempt to wet his lips with his tongue.
– After the initial set, the rim was examined; excess trimmed under extension corrected and placed back in mouth and molded.
– The occlusal rim is duplicated in wax with the help of silicone putty buccal and lingual indices. The tentatively completed wax neutral zone rim is ready.
– Wax is softened on the mandibular rim, it is placed back in the mouth and the mandible is carefully guided into centric relation.
– Excess wax was trimmed, the remaining wax was softened and the patient was instructed to swallow without guidance.
– Anterior teeth were selected for esthetics and semi- anatomic posterior teeth rather than non- anatomic posterior teeth were selected in an attempt to stabilize occlusion in the maximal intercuspal position and improve mastication.
– The mandibular posterior teeth were positioned in the recorded neutral zone and special care was taken to preserve the form of the polished surface.
– Because of the unfavourable relationship between the maxillary and mandibular residual ridges, and to avoid any violation of the recorded neutral zone, a reverse articulation occlusion scheme was developed in the left molar area.
– The dentures were processed, finished & polished and delivered.
– The most important benefit of this procedure was the immediate improvement in the oral function due to the passive and active muscular fixation of the mandibular denture.
Multiple suction cup dentures
Arthur C. Jermyn
JPD 1967; 18; 316-25
A basic concern of edentulous patients is retention of their dentures. This has led to considerable research. The use of multiple miniature suction cups made from a soft material lining the denture satisfies the requirements of retention and stability.
INDICATIONS
1. desire on part of the patient for extra retention and stability
2. in cases of extremely resorbed ridges
3. palateless dentures
4. knife-edged and flat ridges.
CONTRAINDICATIONS
1. presence of moniliasis in the mouth
2. allergy to silicone liners
TECHNIQUE
– the tissues should be healthy before an impression is made for new set of dentures, or the optimum dentures of the patient may be rebased. Final impression is made in rubber base material.
– Laboratory procedures:
a. casts are poured in artificial stone of medium hardness.
b. In order to use the special drill, it is necessary to prepare the stone casts for easy access. The lingual surfaces of the lower cast are cut away and the borders are trimmed to allow the drill to cut the stone at right angles to the surface.
c. The special suction cup drill is basically a trephine with ten cutting teeth. It has a threaded shank that fits into a screw-type handpiece.
d. The ideal depth of the cut in the stone varies from 0.010 of an inch to 0.015 inch, depending on the type and depth of the tissues.
e. Suction cup holes should never be drilled over frenum attachments, and they should be kept away from the denture borders by at least 2 mm.
f. The holes should be drilled with a definite planned outline. The holes are spaced 1.0mm to 1.5 mm apart, so the silicone cup edges will not overlap each other when they would be compressed against the soft tissues.
g. A butt joint between the silicone liner and the hard acrylic resin is preferable to simplify trimming and polishing.
h. The butt joint is also necessary to act as a seal around the entire border during the packing of the silicone material. It serves to contain the silicone and forces the soft material into the suction cup holes, filling them completely.
– Placement of unusual denture
a. the new dentures are soaked in the fungicide solution for at least 15 minutes and then rinsed with clear tap water before being placed in the patient’s mouth.
b. The patient is asked to maintain a closing pressure on the dentures for several minutes in order to allow the suction cups to flare out and partly settle into the tissues.
c. Any occlusal discrepancies are then corrected. Follow up regime is set for further adjustments of discrepancies.
d. Patient is asked to leave the dentures out of the mouth during sleep.
One of the most consistently frustrating areas of maxillofacial rehabilitation of edentulous patients who have had radical cancer surgery of the tongue, floor of the mouth and mandible. Mandibulectomy and commando procedures involve extensive loss of tissues and associated functions.
ปั้มไลค์
24 Jul 2020Like!! Thank you for publishing this awesome article.